Blood Perfusion Effect of Acupuncture on Acute Facial Paralysis Observed by Laser Speckle Technique
2014-06-19ZhongWeizhengCuiHan2ChenYi2YangZhuoxin3YuHaiboRaoXiaodan
Zhong Wei-zheng, Cui Han2, Chen Yi2, Yang Zhuo-xin3, Yu Hai-bo, Rao Xiao-dan
1 Shenzhen Hospital of Traditional Chinese Medicine, Shenzhen 518033, China
2 Institute of Biomedical and Health Engineering, Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, Shenzhen 518055, China
3 Shenzhen Maternal and Child Health Care Hospital, Shenzhen 518045, China
CLINICAL STUDY
Blood Perfusion Effect of Acupuncture on Acute Facial Paralysis Observed by Laser Speckle Technique
Zhong Wei-zheng1, Cui Han2, Chen Yi2, Yang Zhuo-xin3, Yu Hai-bo1, Rao Xiao-dan1
1 Shenzhen Hospital of Traditional Chinese Medicine, Shenzhen 518033, China
2 Institute of Biomedical and Health Engineering, Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, Shenzhen 518055, China
3 Shenzhen Maternal and Child Health Care Hospital, Shenzhen 518045, China
Author: Zhong Wei-zheng, bachelor, attending physician.
E-mail: roade@163.com
Objective: To observe effect of acupuncture for acute facial paralysis patients with ocular skin blood perfusion, and to explore the safety and effectiveness of acupuncture in treating acute facial paralysis.
Methods: Thirty patients with acute facial paralysis were enrolled and acupunctured in facial points and bilateral Hegu (LI 14), and the PeriCam laser speckle flow video monitoring system was used not only for recording ocular skin blood perfusion condition in both normal and affected sides before acupuncture, at 15 min after acupuncture and after removing needles immediately, but also for calculating reduction ratio of ocular skin average perfusion in the affected side face compared with the healthy side.
Results: Compared with the healthy side of face, the ocular skin blood perfusion of the affected side after acupuncture was significantly different from that before intervention. The blood perfusion levels after 15-minute acupuncture and at the time of remaining needles were significantly different from the basic line (allP<0.01).
Conclusion: Acupuncture can significantly improve eye blood perfusion of the acute facial paralysis, enhance metabolic activity of the affected facial tissues, and promote the recovery of facial nerve function.
Acupuncture Therapy; Facial Paralysis; Bell Palsy; Perfusion; Blood Circulation
Facial paralysis is one of the common diseases in acupuncture clinic, and many clinical reports have shown that acupuncture is significantly effective for facial paralysis and more effective than conventional Western medicine[1-2]. According to years of clinical studies, the majority of acupuncture doctors believe that the best time for acupuncture intervention for facial paralysis is during the acute phase. The earlier acupuncture intervenes, the better efficacy there is and the shorter the treatment course is[3-5]. However, some doctors still doubt whether acupuncture intervention in acute phase will aggravate nerve damage. And strong evidence in clinical acupuncture has been absent regarding that what effect acupuncture produces in acute phase. By using the PeriCam PSI system (laser speckle blood perfusion video monitoring system), we observed the facial microcirculation improvement in facial paralysis of acute stage after acupuncture thus to seek the objective evidence of acupuncture in treating this disease during acute phase. Now, the report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
On the base of the diagnostic criteria of Bell's facial paralysis inScience of Acupuncture and Moxibustion[6]andClinical Neurology[7], diagnostic criteria were formulated as follows: an acute onset and a history of exogenous pathogen invading face such as cold, wind;the affected side of the face shows stiff muscles, numbness and paralysis, the wrinkles of forehead disappear, rima oculi enlarges so as to expose eyeball and increase tears secretion, nasolabial fold becomes shallower, mouth corner droops and twists to the contralateral side; the affected side of face cannot frown, knit brows or close eye completely, and cannot show teeth, pouch cheek or whistle properly; there also may be ear pain, taste sensitivity of the posterior 2/3 of the tongue diminishes or disappears, and hyperacusis or hearing disorders.
1.2 Inclusion criteria
Met the above mentioned diagnostic criteria; 15-50 years old; disease duration ≤7 d; volunteered to participate in the study and signed informed consent forms.
1.3 Exclusion criteria
Failure to meet the inclusion criteria; face paralysis was caused by other diseases; without other serious diseases affecting the implementation of the treatment.
1.4 General data
Thirty outpatients with peripheral facial paralysis were enrolled from the Acupuncture Department of Shenzhen Hospital of Traditional Chinese Medicine from January to October 2013, and their ages ranged from 23 to 50 years old with an average age of (33±4) years, including 16 males and 14 females with 1-7 d duration, and none of the patients had received any treatment of Western or traditional Chinese medicine. There was no dropout case in treatment process.
2 Acupuncture Methods
Points: Cuanzhu (BL 2), Yangbai (GB 14), Taiyang (EX-HN 5), Sibai (ST 2), Quanliao (SI 18), Dicang (ST 4), Jiache (ST 6), Yingxiang (LI 20), and Yifeng (TE 17) on the affected side, and bilateral Hegu (LI 4).
Operation: Stainless steel needles of 0.3 mm in diameter and 25 mm or 40 mm in length were used. Inserted the needles subcutaneously downwards into Cuanzhu (BL 2) and Yangbai (GB 14) for 0.3 cun;inserted the needle perpendicularly upwards into Taiyang (EX-HN 5) and Quanliao (SI 18) for 0.3 cun;inserted subcutaneously upwards into Sibai (ST 2) for 0.3 cun; inserted the needle from Dicang (ST 4) toward Jiache (ST 6) for 1 cun, and also from Jiache (ST 6) toward Dicang (ST 4) for 1 cun; inserted obliquely into Yingxiang (LI 20) along nasolabial fold for 0.2 cun; inserted perpendicularly into Yifeng (TE 17) and Hegu (LI 4) for 0.5 cun. After qi arrival, retained needles for 30 min, and manipulated the needles every 10 min gently. The treatment was given 5 times per week with 2 d rest between 2 weeks and therapeutic efficacy was observed after 4 weeks.
3 Result Observations
3.1 Observation conditions and environment
Observation room was quiet and comfortable with low noise and soft lights, its temperature maintained at 23-26 ℃, and humidity between 45% and 50%.
3.2 Equipment
PeriCam PSI system manufactured by Perimed AB was used. This system is based on laser speckle contrast analysis (LASCA) technology, and can monitor a large area of tissue perfusion by real-time dynamic imaging. With high spatial and temporal resolution, this system can monitor the region perfusion up to 100 fps by 1 388 × 1 038 pixel CCD camera laser detection. After the computer’s process, the photographs taken by the camera will be displayed as a perfusion map on the screen. There is also a color camera used to record the behavior of the measured object, color photographs and perfusion image shows the same area, which can assist to determine whether the object is moving during monitoring process, in order to help blood perfusion volume and intensity image evaluation. In addition to real-time display more than two monitoring images, the PIMSoft program analysis function also can perform statistical analysis of the perfusion area in a freely defined region of interest (ROI). The instrument uses a laser wavelength of 785 nm as a monitoring light source with maximum output power of 70 mW, which is in line with the relevant safety standards of IEC 60825-1: 2007 class I requirements. The instrument is class 2A medical devices and compliance with medical devices MDD 93/42/EEC authentication requirements. During facial monitoring, no special protection is required but only closing eyes.
3.3 Operating methods and statistical analysis
PeriCam PSI system was used to record blood perfusion data during patients’ first acupuncture treatment for statistical analysis. Because of thin skin and rich blood flow, the eyes were selected as ROI to reflect the facial blood flow. Patients entered the investigation room, lying 10 min on the couch quietly with eyes closed and same head posture in a stereotypes pillow. The lens was placed just 13-18 cm above the patient's face, and then acupuncture asbefore. The blood flow images of the ocular skin were recorded and numbered at three time points: before acupuncture, 15 min after acupuncture and right after needles were removed. At each time point, monitoring lasted about 2 min. The stable intermediate data were selected to analyze, and the head and tail instability data were removed. During the observation, the patient kept stable emotion and relaxed eye which was to naturally close eyes to keep eye balls stationary.
PIMSoft was used for collecting ocular blood perfusion images (Figure 1), ROI blood perfusion curve (Figure 2) and ROI% change table. At each time point, the ROI average blood flow of contralateral ocular skin was taken as a reference value (reference, ref), and reducing ratio of average ocular skin blood perfusion of the affected side compared with the healthy side was calculated (ROI%) by the following formula: ROI% = (ROI value of the affected side -ROI value of the healthy side) ÷ ROI value of the healthy side × 100%.
The measurement data were expressed as mean ± standard deviationanalyzed by independent samplet-test, and the SPSS 21 version software package was used for statistical analysis.
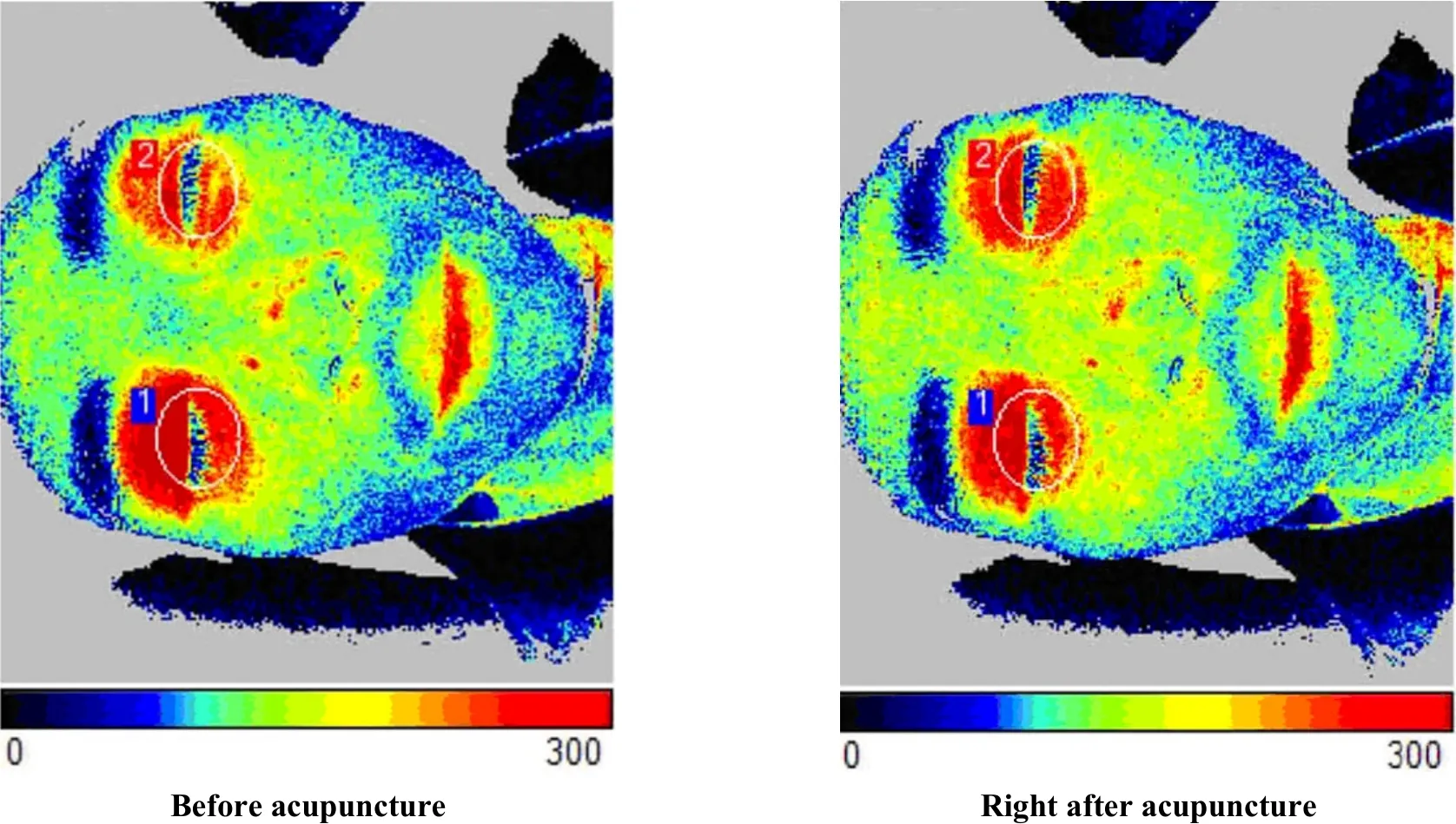
Figure1. Facial blood perfusion images before and after the first acupuncture(areas in the circle stands for ROI, 1 is the image of the healthy side and 2 is the image of the affected side)
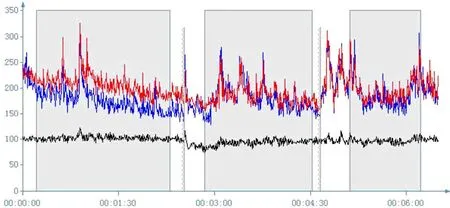
Figure 2. ROI blood perfusion curve during the first acupuncture treatment (the red line stands for the healthy side, blue line stands for the affected side, and black line stands for the average blood flow value of the whole face)
3.4 Therapeutic effect criteria
Referring to House-Brackmann (H-B) facial nerve function evaluation and classification method recommended by the Fifth International Symposium on Facial Nerve Surgery[8], the therapeutic effect criteria were formulated as follows:
Recovery: Function of the facial nerves innervation areas return to normal.
Markedly effective: Functions are slightly weakened or consequential movement may be found after careful observation; face is symmetrical when stationary; moderate movement on the forehead, eyes can be completely closed using light force, and mouth shows slightly asymmetrical.
Effective: There is obviously weakened function but no damage of bilateral asymmetry, and parasitic motion, contracture, and (or) hemi-facial spasm also can be observed; there is weakened movement on the forehead, eyes can be closed completely by hard force, mouth corner can be forced to move, and mouth is obviously asymmetrical.
Invalid: Face is asymmetrical when stationary, forehead cannot be moved, eyes cannot be completely closed; only mouth can be slightly moved.
3.5 Results
Before acupuncture, ROI% was (-15.73±11.06);15 min after acupuncture, ROI% was (-7.12±7.28), which was significantly different from that before treatment (P<0.01), indicating that blood perfusion increased after acupuncture. Right after the needles were removed, ROI% was (-2.43±6.85), which was significantly different from that before treatment (P<0.01), showing that blood perfusion on the affected side continued to increase.
After 4 weeks treatment, 18 cases were recovery, 7 cases were markedly effective, 2 cases were effective, and 2 cases were invalid, and the total effective rate was 93.3%.
3.6 Case study
A 35 years old male patient firstly visited the clinic on March 25, 2013.
Chief complaint and history of present illness: The left eye-mouth deviation for 3 d without any treatment.
Symptoms: The left incomplete eyelid closure with increased tear secretion, mouth was crooked to right, food was stuck between the teeth and the left cheek, posterior of ear was painful, and there was no taste loss or hyperacusis.
Examination: Dark and pale tongue with thin and white coating, and tight pulse. Left rima oculi slightly enlarged with incomplete eyelid closure, the wrinkles on the forehead disappeared, left nasolabial fold became shallower, mouth corner is crooked to right, air in mouth leaked when cheek pouched, light tenderness behind the ear, and the right facial motor and sensory function were normal.
Diagnosis of traditional Chinese medicine: Facial paralysis (wind-cold obstructing the collaterals).
Diagnosis of Western medicine: Left facial neuritis.
Treatment process: Conducted acupuncture treatment as described above and applied PeriCam PSI with dynamically observing the ocular skin blood perfusion changes at the 3 time points during treatment process. Making the ocular skin blood flow in the healthy side as a reference value, before acupuncture, ocular skin blood flow on the affected side was -16.2%, it was -5.35% after 15-minute acupuncture, and it was 0.64% right after needles removed (Table 1). This patient received five times of treatment per week, and he was totally cured after 4 consecutive weeks treatment.
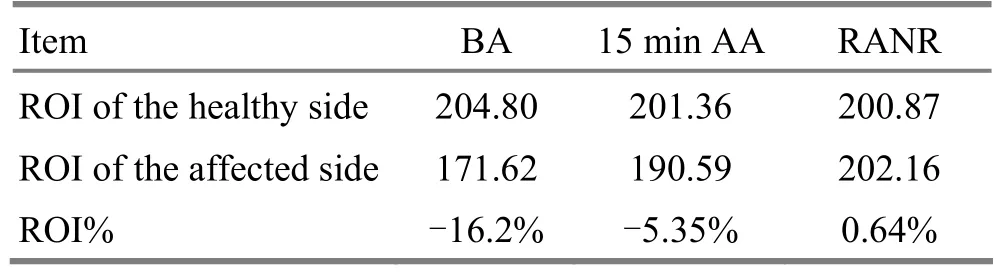
Table 1. ROI values changes before and after acupuncture (PU)
4 Discussion
It is believed in Traditional Chinese medicine that the facial paralysis results from obstruction of qi and blood and dystrophy of tendons and muscle caused by exogenous cold, wind and heat. Alternatively, it can be induced by qi and blood movement disorder caused by a weak constitution, insufficiency vital qi, emptiness of collaterals, weakened Wei-defensive qi as well as exogenous pathogen invasion in the face[9-11]. In addition, it’s confirmed in modern medicine that facial paralysis is caused by facial nerve palsy, and noted that the blood supply condition of the facial nerve directly affects the facial nerve function[12]. Thus, the facial nerve infection, catching cold or other factors can affect the facial microcirculation and finally lead to facial paralysis. This shows that both Chinese and Western medicines consider the key of diagnosis and treatment of facial paralysis is facial microcirculation. Previous studies of acupuncture treatment on facial paralysis stay in clinical observation, and there still lacks in-depth mechanism research for it. In recent years, with the development of monitoring technology, many methods to display perfusion have become important means to show acupuncture effect, such as thermal infrared imaging, laser Doppler, laser speckle imaging.
Some studies have shown that acupuncturing Hegu (LI 4) of healthy people can improve facial blood perfusion[13-15]. In this study, we simultaneously acupunctured both points in the face meridians and Hegu (LI 4) chose by the majority of acupuncture doctors with PeriCam PSI real-time monitoring in order to observe dynamic changes of blood perfusion in the affected and healthy sides of face before, during and after acupuncture, and the results showed that acupuncture could significantly increase the affected side’s eye blood perfusion, which meant its facial tissue metabolic activity increased and played a significantly important role in restoring facial nerve function. In acute phase of facial paralysis, because facial nerves are in inflammation and edema condition, it’s possible and understandable that the damage may spread and the disease may appear worsening trend. However, it is important to promptly improve facial blood circulation, promote inflammation and edema absorption, and relieve nerve compression to prevent further damage to the facial nerve, and appropriate acupuncture treatment can achieve these effects. Our study has provided a strong evidence for the safety and effectiveness of acupuncture in treating acute facial paralysis. Thus, in the acute phase of facial paralysis, acupuncture treatment is effective and necessary, and it will not aggravate disease condition. However, large sample studies are still needed and acupuncture effect differences on different classification also need further exploration.
Conflict of Interest
The authors declared that there was no conflict of interest in this article.
Acknowledgments
This work was supported by 2012 Shenzhen City Key Laboratory Program in Area of People's Livelihood: Acupuncture Laboratory for Modern Application and Research.
Statement of Informed Consent
All the patients knew this study and signed the informed consent.
[1] Xiang GW. Clinical observation on treating 100 cases of peripheral facial paralysis by acupuncture combined with moxibustion. CJCM, 2012, 4 (22): 37-38.
[2] Deng SF. Clincial observation of peripheral facial paralysis treated by combination acupuncture therapy. Zhongguo Yiyao Daobao, 2012, 14(11): 1905-1906.
[3] Yang G, Zhang ZL, Yang JG, Ge SH, Ge JK, Gao JF, Zhu LW, Zhang SP, Chen SW, Dong SH, Lu MH, Yang ZF. When is the best time for acupuncture intervening in facial paralysis treatments? Zhongguo Zhenjiu, 2005, 25(8): 555-556.
[4] Shen TL, Cao LY, Zhang W, Li Y, Wu QH, Yao MJ, Gu LY. Clinical study on acupuncture intervention time for treatment of peripheral facial paralysis. Zhongguo Zhenjiu, 2009, 29(5): 357-360.
[5] Yan NW. Acupuncture intervention effect for acute facial neuritis. Heilongjiang Zhongyiyao, 2012, (5): 44-45.
[6] Shi XM. Science of Acupuncture and Moxibustion. Beijing: China Press of Traditional Chinese Medicine. 2002: 225.
[7] Huang RX, Liang XL, Liu ZL. Clinical Neurology. Beijing: People’s Medical Publishing House, 1996: 201.
[8] House JW. Facial nerve grading systems. Laryngoscope, 1983, 93 (8): 1056-1069.
[9] Tian LL. Brief discussion on ancient doctors’ knowledge of the etiology and pathogenesis of peripheral facial paralysis. Xiandai Zhongxiyi Jiehe Zazhi, 2010, 19(15): 1874.
[10] Wei Y, Kou JY. Evaluation of the efficacy of acupuncture in treating peripheral facial paralysis based on orthogonal experimental design. Shanghai Zhenjiu Zazhi, 2011, 30(12): 830-832.
[11] Li SP, Huo GM, Li JD, Sun D. Therapeutic effect analysis on combined acupuncture and medication for peripheral facial paralysis. J Acupunct Tuina Sci, 2011, 9(3): 185-187.
[12] Michael J. Blunt, the blood supply of the facial nerve. J Anat, 1954, 88(Pt 4): 520-526.
[13] Gu X. Dynamic observation of the influence of point Hegu acupuncture on magnetoencephalogram. Shanghai Zhenjiu Zazhi, 2005, 24(7): 38-40.
[14] Tian YY, Huang T, Wang GJ, Jia SY, Zhang WB. Observation on acupuncturing Hegu (LI 4) for facial different areas blood perfusion by laser speckle technique. Zhongguo Zhongyi Jichu Yixue Zazhi, 2013, 19(2): 183-184.
[15] Xu JY, Yan B, Wang W, Hao JD, Lu N, Li K, Shan BC. Cerebral function imaging research on the after-effect of point Hegu acupuncture. Shanghai Zhenjiu Zazhi, 2005, 24(10): 33-36.
Translator:Deng Ying
R246.6
: A
Date:February 15, 2014
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Observation on Clinical Effects of Tuina plus Hot Compress for Infantile Diarrhea Due to Spleen-kidney Yang Deficiency
- Clinical Study on Point Application Using Chinese Herbal Medicine for Pediatric Chronic Cough
- Therapeutic Effect Observation on Combining Electroacupuncture and Tuina for Migraine
- Therapeutic Efficacy Observation on Combined Taijiquan and Auricular Point Sticking for Perimenopausal Insomnia
- Clinical Study on Fu’s Subcutaneous Needling with Laser for Postherpetic Neuralgia
- Therapeutic Efficacy of Tuina in Treating 48 Cases with Knee Osteoarthritis
