Post-pancreaticoduodenectomy hemorrhage:risk factors,managements and outcomes
2014-06-11
Beijing,China
Introduction
Over the past two decades,operative mortality rate after pancreaticoduodenectomy (PD)has declined below 5% in most high-volume centers,[1-3]but the morbidity still remains as high as 30%-50%.[4-7]The most frequent major complications after PD are pancreaticfistula,delayed gastric emptying,intra-abdominal abscess and post-PD hemorrhage(PPH).PPH is a less frequent but severe complication after PD with 2.5%-20.2% incidence and 11.0%-56.2%related mortality.[4-16]PPH can be classified into early PPH (occurring in the first 24 hours postoperatively)and late PPH (after 24 hours of operation).[17]
Early PPH is usually due to some surgical mishap,[6,8,18-20]while late PPH is often related to pancreaticfistula and intra-abdominal abscess.[7,10,13]The best treatment of the early PPH is urgent reoperation.Over the past several years,endoscopy and angiography,not surgery are the standard treatment for late PPH.Despite the recent advances in diagnosis and treatment of PPH,such as spiral CT arteriograpy and transarterial technology,the prognosis of PPH remains poor.Thus,prevention of PPH after pancreatectomy seems to be more important.However,no validated preventive measures are available for the control of this severe complication.
This study was to identify the risk factors of PPH and report our experiences in the management of the complication.
Methods
A total of 840 cases of PDs (550 males and 290 females)which had been performed from 2000 to 2010 were analyzed.All of the PDs cases were from the Institute of Hepatobiliary Surgery of the Chinese PLA General Hospital (Beijing,China).The median age of the patients was 54 years (range 4-81).Indications for PD were malignant disease in 88.5% and benign or borderline tumors in 11.5%.
Surgical technique and perioperative management
In our center,prior to the operation (within 3 days before operation),we routinely measure the patients' white blood cell,hemoglobin,platelet,alanine aminotransferase,serum total bilirubin (TB),plasma albumin and prothrombin time.When the serum TB >171 μmol/ L,vitamin K is routinely given preoperatively to the patients,while preoperative biliary drain is not routinely performed.
Laparotomy was performed through a right subcostal reverse L incision.The operative procedure was the modification of pylorus-preserving pancreatoduodenectomy (PPPD) or conventional PD,i.e.Whipple's operation based on the extent of tumor and lymph node of pylorus involvement.Veins involvement is not a contraindication for PD.Before 2006,all surgeons used electrome to cut the pancreas,but now increasing surgeons tend to cut the pancreas with surgical knife and then use electrocoagulation for hemostasis of the pancreatic cut surface.Selection of types of pancreaticojejunostomy (PJ) was based on the diameter of the pancreatic duct,pancreas parenchyma and surgeon's experience.Usually,three methods are used to accomplish PJ after PD:end-to-side,two layer,duct-to-mucosa PJ (n=670); end-to-end,two layer,invagination PJ,i.e."dunking" the pancreatic remnant into the jejunum (n=77); and end-to-side,two layer,invagination PJ (n=44).The routine procedure for reconstruction of the alimentary continuity was the classical method during which one jejunum loop was used.In the construction of using two independent jejunum loops,one was used to fashion the pancreatic and biliary anastomosis and the other was used for gastric anastomosis in only 48 patients.A pancreatic duct stent was used in the PJ in accordance with the diameter of the pancreatic duct and surgeon's experience,and the stenting included external pancreatic duct stenting in 457 patients,internal in 220,and no stenting in 63.The anastomotic areas of both the PJ and biliary anastomosis were drained separately with open drains.
The onset,location and severity of hemorrhage were classified according to the International Study Group of Pancreatic Surgery (ISGPS).[17]Early PPH was defined as hemorrhage within 24 hours after surgery and late PPH,24 hours later after operation.The location,intraluminal or extraluminal and severity,mild or severe,were based on different clinical parameters and intervention was required.Three different grades of PPH (grades A,B,and C) were defined according to the time of onset,the site of bleeding,severity,and clinical impact.
Pancreaticfistula was defined by the following criteria proposed by ISGPS:[21]any measurable volume of drain fluid within 3 days after operation,the amylase content of drain fluid was 3 times greater than that of the upper normal serum value.In our center,the content of drain fluid is routinely measured on day 3 after operation.According to the clinical impact on the patient,pancreaticfistula can be graded into A,B or C.Intra-abdominal abscess was diagnosed according to the following criteria:persistent fever,elevated white blood cells and intra-abdominal fluid collection identified by ultrasonography or computed tomography with positive culture.[22]Postoperative mortality refers to the rate of death in hospital after PD.
Statistical analysis
Statistical analysis was performed with SPSS 18.0.Continuous variables were presented as mean±SE or median and 95% confidence interval and compared by using Student's t test,the Mann-Whitney U test or Wilcoxon's signed-rank test,as appropriate.The Chisquare test or Fisher's exact test was used to compare categorical variables.Logistic regression multivariate analysis was carried out to determine independent risk factors for PPH.Results were presented as odds ratios(ORs) with 95% confidence intervals (95% CIs).P<0.05 was considered statistically significant.
Results
In this series,the overall morbidity rate and mortality rate were 36.3% (305/840) and 3.3% (28/840),respectivery.PPH occurred in 73 patients (8.7%),and 4 patients were classified into grade A,51 into grade B,and 18 into grade C.In addition,167 patients (19.9%) developed pancreaticfistula and 31 (3.7%) had intra-abdominal abscess.
Among the 73 patients with PPH,59 were male and 14 female,ranging from 21 to 77 years with a median age of 55.4.The median postoperative hospital stay was 35.4 days (range 5-158).Nineteen patients suffered from early PPH and 54 from late PPH.Twenty-eight patients had intraluminal hemorrhage,and 33 had extraluminal hemorrhage,and 12 had both.The initial presentation of bleeding was as follows:blood loss via nasogastric tube (26.0%,19/73),hematemesis (13.7%,10/73),melena or hematochezia (9.6%,7/73),"T" tube bleeding (1.4%,1/73),and blood loss from abdominal drains (49.3%,36/73).The origins of hemorrhage,verified by endoscopy,angiography and relaparotomy are summarized in Table 1.
Risk factors
The risk factors for PPH were classified into three broad categories:(1) preoperative factors:patient age,gender,body mass index (BMI),weight loss,comorbidities,abdominal operation history,preoperative serum TB,preoperative biliary drain(PBD) and duration of PBD; (2) intraoperative factors:type of resection,operative time,estimated blood loss,intraoperative blood transfusions,pancreatic duct,pancreatic duct stenting,post biliary drain,extent of lymph node resection,reconstruction of blood vessels and type of pancreatic anastomosis; (3) postoperative factors:postoperative pancreaticfistula,bile leakage,intra-abdominal abscess and pathologic findings.Some data were missing,so the denominators within each group did not reach 840.
In our institute,PD cases have rocketed yearly since 2004; however,the PPH rate has not changed (P=0.35,χ2test; Fig.1).
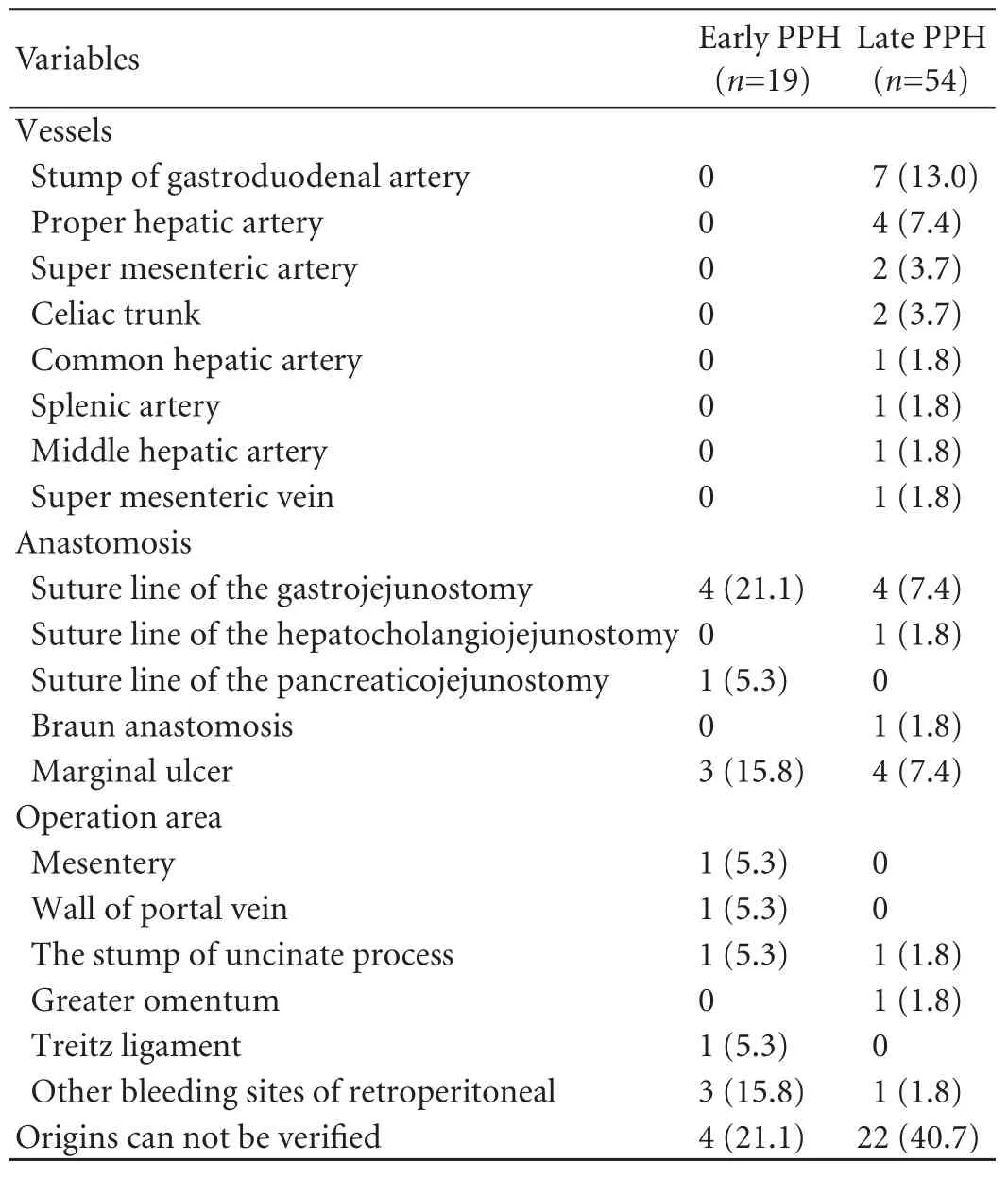
Table 1.Origins of bleeding (n,%)
Univariate analyses of the preoperative factors for early PPH and late PPH are summarized in Table 2.Age and BMI were not correlated with early or late PPH rate.Male gender was correlated with late PPH (83.3%vs 64.0%,P=0.01).About the comorbidities,only diabetes mellitus was related to late PPH rate (20.4% vs 9.1%,P=0.01).An abdominal operation history would increase the complexity of operation and therefore,might increase the risk of PPH.Our study revealed that abdominal operation history significantly increased the risk of both early and late PPH (89.5% vs 20.1%,P<0.01;83.3% vs 15.6%,P<0.01).Preoperative (within 3 days)serum TB levels did not affect either early or late PPH.Among 291 patients with TB level of more than 171 μmol/L on admission,126 underwent PBD.However,this procedure and its duration had no in fluence on early or late PPH (P=0.40 and 0.92,respectively).
Among intra- and postoperative factors (Table 3),the operative time and type of PJ were the risk factors for early PPH.The early PPH was higher in patients with end-to-side invagination method compared with other techniques (11.4% vs 1.6% or 1.4%,P=0.00).
The intra- and postoperation risk factors for late PPH included end-to-side invagination pancreaticojejunostomy,diameter of the pancreatic duct,postoperative pancreaticfistula,bile leakage,and intra-abdominal abscess (Table 3).Late PPH occurred in 26 of 160 patients (16.3%) with postoperative pancreaticfistula,7 of 40 patients (17.5%) with bile leakage and 12 of 30 patients (40.0%) with intra-abdominal abscess.All of these complications were correlated with PPH (P=0.00,0.01 and 0.00,respectively).
We compared the complexity of operation and the changes in operative skill of surgeons from 2000 to 2010 (Fig.2).The operative time,estimated blood loss,intraoperative blood transfusion,extended PD and reconstruction of vessels were analyzed.Prolonged operative time was the only risk factor for early PPH.

Fig.1.Longitudinal trends in PD case volume per year,all surgical complications per year,PPH cases per year and rate of PPH.There was a sharp increase in PD case volume per year from 2004,however,no statistically significant change of PPH rates over time was found (P=0.19).
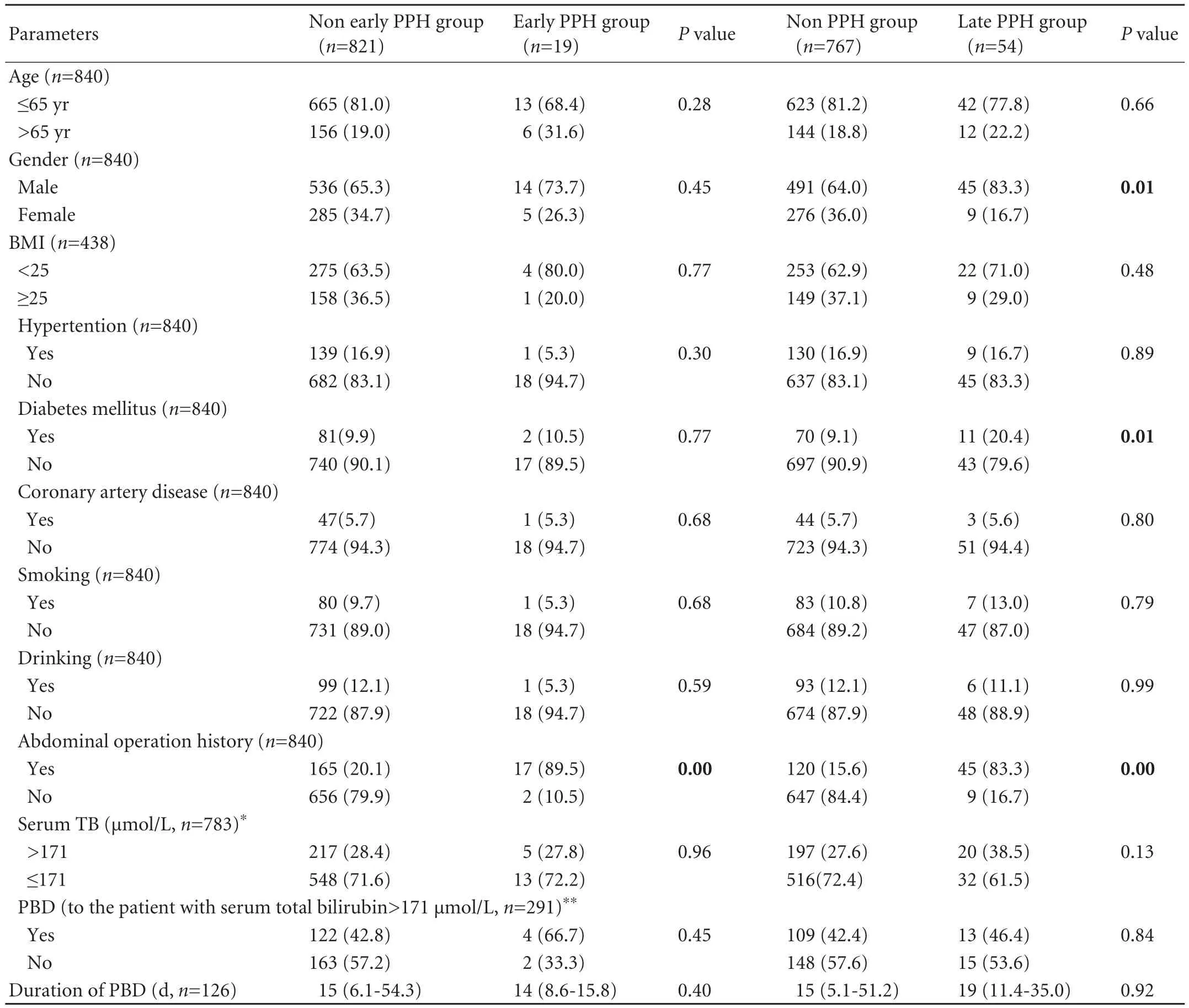
Table 2.Univariate analyses of preoperative factors for early PPH and late PPH (n,%)
Pathological diagnoses are shown in Table 4.Neither malignancy nor benign lesions affected the incidence of early or late PPH.The top three malignant tumors for pancreatectomy in our hospital were Vater's ampullary carcinoma (36.8%),pancreatic ductal adenocarcinoma(22.0%) and distal cholangiocarcinoma (19.0%).Again,tumor type did not affect PPH.
Univariate analysis revealed that there were three risk factors for early PPH and eight for late PPH.These factors were examined separately via a multivariate model (Tables 5 and 6).There was no independent risk factor for early PPH.Male gender (OR=4.40;95% CI:1.34-14.49),diameter of the pancreatic duct(OR=0.64; 95% CI:0.45-0.90),end-to-side invagination PJ (OR=5.65; 95% CI:1.68-19.00),pancreaticfistula(OR=2.33; 95% CI:1.05-5.17),and intra-abdominal abscess (OR=12.19; 95% CI:3.81-39.02) were predictive factors for late PPH.Intra-abdominal abscess was the strongest predictor.
Management
E arly PPH
Four patients responded to conservative therapy.Initial endoscopy of the upper gastrointestinal tractwas performed in three patients,and hemorrhage was successfully controlled in two.Twelve patients received immediate relaparotomy; and the procedure included ligation of bleeding source (n=8),gastrotomy (n=3) and reconstruction of gastrojejunostomy (n=1).

Table 3.Univariate analyses of intraoperative and postoperative factors for early PPH and late PPH

Fig.2.Longitudinal trends in rate of PPH and PD case number per year of five surgeons.Although all surgical volume of the five surgeons increased dramatically from 2004,there was no statistically significant change in the PPH rate (P=0.86,0.63,0.49,0.94,0.67,respectively,χ2 test).
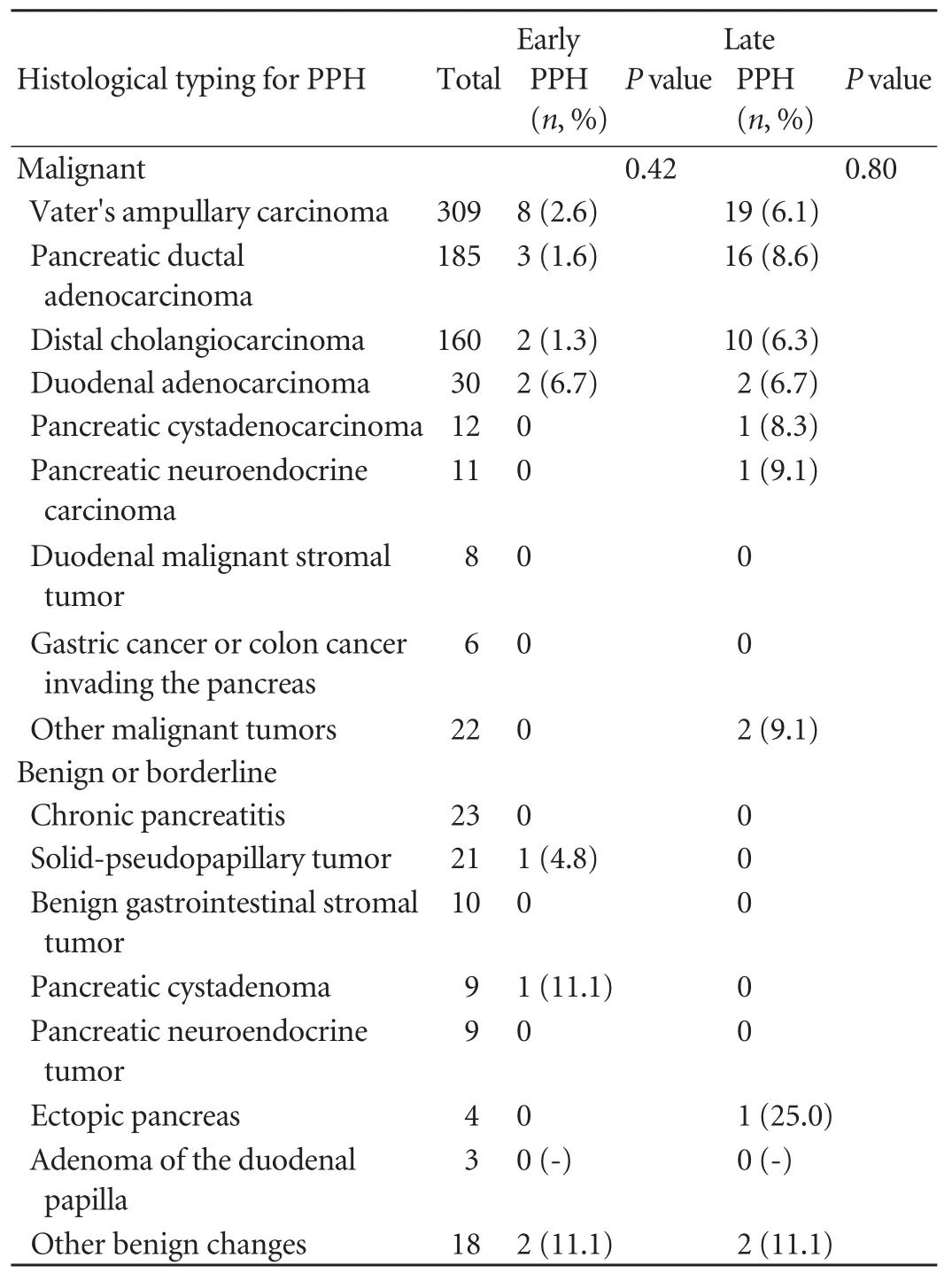
Table 4.PPH based on pathological diagnosis

Table 5.Multivariate logistic regression models of independent risk factors for early PPH (n=624)
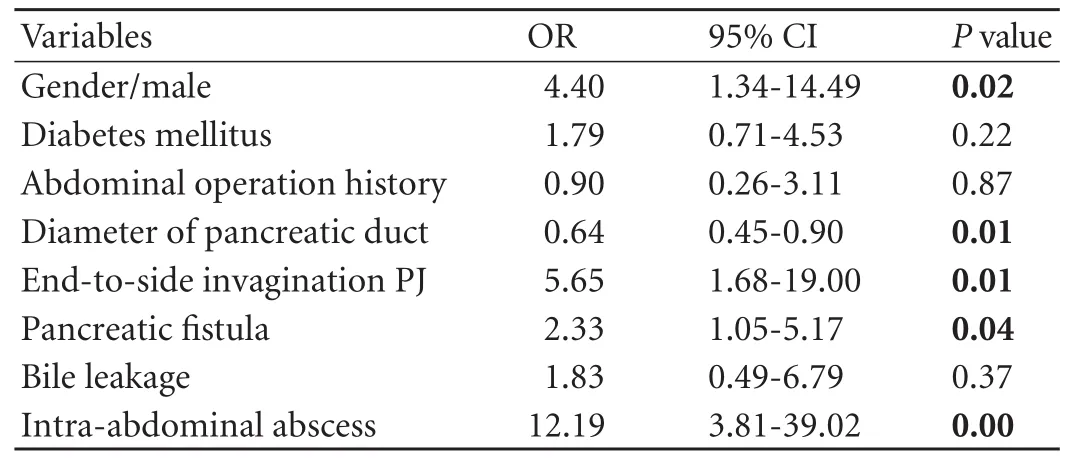
Table 6.Multivariate logistic regression models of independent risk factors for late PPH (n=541)
Late PPH
Fifteen patients (27.8%) responded to conservative therapy.Initial endoscopy was performed in 12 patients(22.2%).The success rate of endoscopic hemostasis was 41.7% (5/12).Bleeding could not be effectively controlled in 7 patients after endoscopy,4 of them received interventional endovascular therapy and 3 relaparotomy.
Initial angiography was performed in 19 patients(35.2%).Selective angiogram revealed pseudoaneurysms in 7 patients,contrast medium extravasation (the signs of active bleeding) in 8,and pseudoaneurysms combined contrast medium extravasation in 2.Thirteen patients were given interventional endovascular treatment,including transartery embolization (TAE) in 11 patients,covered stents placement in 1 and balloon occlusion in 1.In 6 patients,bleeding sources were invisible,and angiography revealed that three had no bleeding but three continued.The immediate success rate of interventional endovascular treatment was 69.2% (9/13).Four patients without hemostasis after interventional procedures underwent relaparotomy.
Rehemorrhage and management
After successful control of hemorrhage,13 patients(17.8%) relapsed.In patients with early PPH,3 had rehemorrhage 3 to 20 days after ligation of the bleeding vessels.The 3 patients subsequently underwent repetitive surgery.
Among the patients with late PPH,rehemorrhage occurred in 6 patients after interventional endovascular therapy.The episode of rehemorrhage after endovascular treatment occurred at 12 hours to 16 days with a mean of 7.6 days.Three patients received repetitive TAE,one underwent reoperation,and the other 2 failed after vigorous treatment.Massive rehemorrhage was seen in 3 patients after relaparotomy,it was not controlled in 2 of them,and the rest one underwent urgent relaparotomy.Rehemorrhage could not be controlled because of poor coagulation,and the patient had extensive hemorrhage from the operative area.The patient died of hemorrhagic shock.Finally,one patient experienced recurrent hemorrhage at 14,24 and 37 days after successful control of bleeding by endoscopy,later a relaparotomy and two TAEs were performed.Unfortunately,the patient died of acute pulmonary embolism.
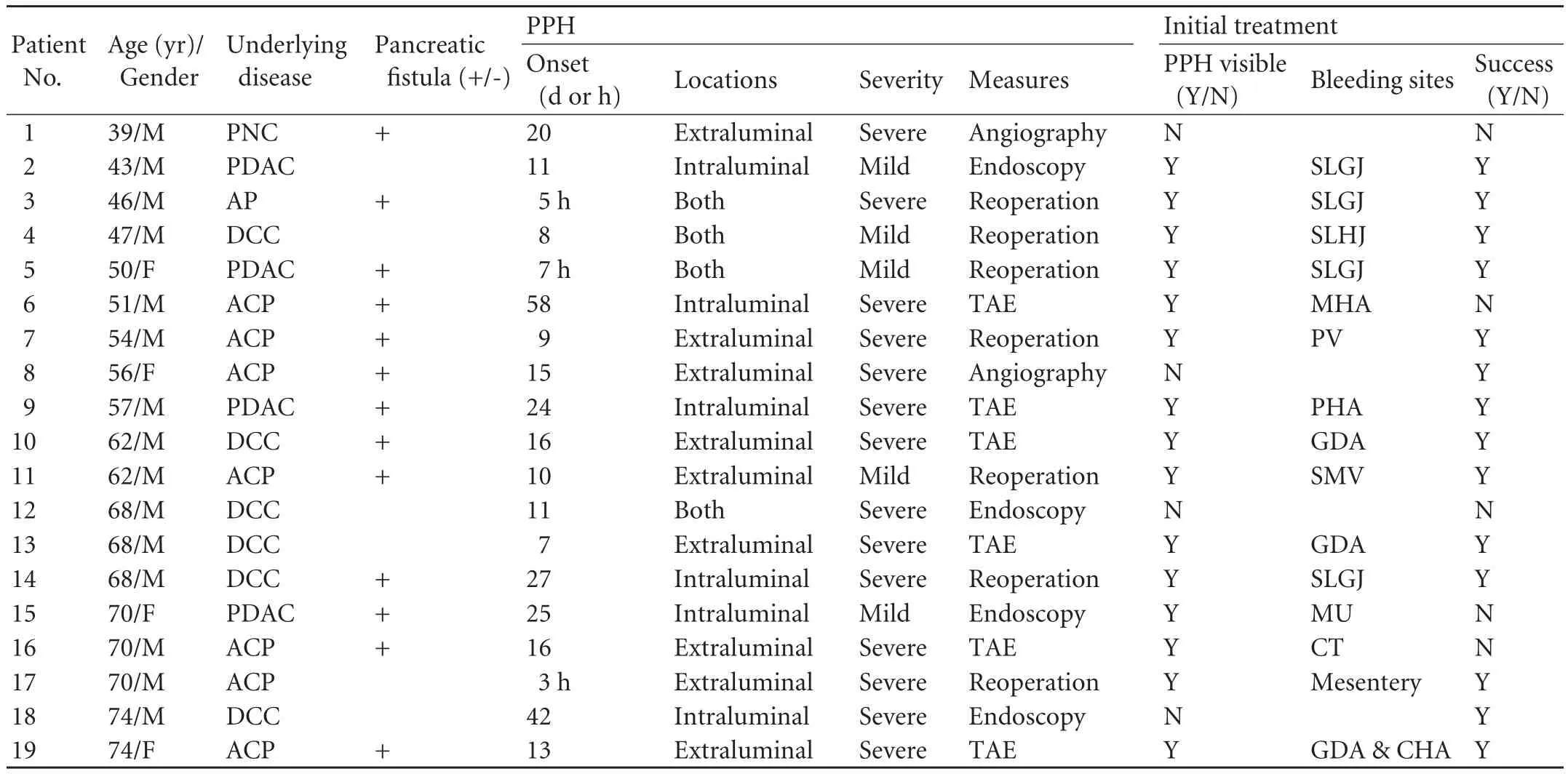
Table 7.PPH characteristics and initial treatment for death cases

Table 8.PPH characteristics and rescue treatment for death cases
Clinical outcome
In our series,54 patients with PPH were cured(74.0%) and 19 (26.0%) died.The mortality rate was 17.6% for patients with intraluminal hemorrhage,27.3%for those with extraluminal hemorrhage and 33.3% for those with both.The outcome revealed that there was no significant difference between early PPH (3 deaths,15.8%) and late PPH patients (16 deaths,29.6%; P=0.38).
Characteristics of dead cases are summarized in Table 7.Eighteen of the 19 patients with lethal outcome were those with malignant diseases,whereas only one patient with benign disease.Nine of the 19 deaths occurred rehemorrhage despite vigorous treatment.Initial hemorrhage was severe in 14 patients but 5 had moderate PPH.Thirteen (68.4%) had pancreaticfistula.Causes of death included hemorrhagic shock complicated with multiple organ failure (n=7),uncontrolled rehemorrhage (n=5),abdominal abscess and sepsis (n=5),hepatic failure (n=1) and pulmonary embolism (n=1).Hemorrhagic shock was a significant factor of mortality.Rebleeding was another significant risk factor of death (9/13 vs 10/60,P<0.01).
Discussion
PPH is still a challenge.The present study analyzed some of the risk factors for PPH in a big cohort,but no independent risk factor for early PPH was found.Since early PPH is thought to be caused by intraoperative technical mishap,[6,8,18-20]surgeons should be familiar with regional anatomy and have adequate surgical skills to avoid the occurrence of early PPH.
Male gender,diameter of the pancreatic duct,end-to-side invagination PJ,pancreaticfistula,and intra-abdominal abscess were the independent risk factors for late PPH.Although the surgical skills of surgeons improved with accumulated experiences,the PPH incidence was not decreased significantly.The complexity of the operation may be related to the incidence of PPH,but this study did not support this hypothesis.It is well known that pancreaticfistula and intra-abdominal abscess are independent risk factors for late PPH.In the present study,48.1% of patients with late PPH had pancreaticfistula.
We found that male patients had a greater risk of PPH.No studies have demonstrated this phenomenon and the mechanism is unclear.In our study,patient number and P value indicated that type I error may be contributive.PJ contributed significantly to PPH in our study.Some authors[23,24]compared endto-side invagination PJ with duct-to-mucosa PJ in pancreaticoduodenectomy.Bassi and colleagues[23]found no difference in postoperative complications.Berger and coworkers found that end-to-side invagination PJ was better than duct-to-mucosa PJ.[24]The present study demonstrated that end-to-side invagination PJ was an independent risk factor for PPH.Another finding of this study was that the small diameter of the pancreatic duct was an independent risk factor for late PPH.The increased size of the pancreatic duct before surgery was a protective factor for PPH.Studies revealed that the diameter of the pancreatic duct is an independent risk factor for post-PD pancreaticfistula which has been confirmed as an independent risk factor of PPH.The thickness of the pancreatic duct is another factor of late PPH.
PPH is classified into early and late onset.ISGPF defined 24 hour as a cut-off line.[17]Because of the difference of pathogenesis of early and late PPH,the treatment is different.We found that early PPH is mainly due to the non-secured ligation of vessels,such as suture line of gastrojejunostomy or areas of resection,but late PPH mainly originates from the erosion or pseudoaneurysm of major arteries.Thus,early PPH,if not treated conservatively,should be treated with urgent relaparotomy and tight ligation of active bleeding site.Unlike early PPH,the late PPH,since the patients always have concurrent or subsequent pancreaticfistula or intra-abdominal abscess,the treatment is more troublesome.Before 2000,there were many controversies over the optimal treatment of late PPH.[4,19,20]However,endoscopy and angiography,not surgical approach,are currently the standard initial management of late PPH,whereas surgery is a therapeutic option under the following conditions:failure of endovascular or endoscopic hemostasis; extraluminal bleeding from the vein system such as the portal vein and its tributaries;and patients with minor bleeding but abdominal abscess or pancreaticfistula required laparotomy treatment.Over one-fifth of our patients with late intraluminal PPH underwent endoscopy and the success rate was 41.7%.Angiographic treatment as initial treatment was applied to 19 patients (35.2%) with late extraluminal PPH and the success rate was 69.2% (9/13).Only 14.8%patients required laparotomy as an initial treatment to control the hemorrhage.
Rehemorrhage,as a poor prognostic factor for PPH,was closely associated with pancreaticfistula.In this series,13 patients had rehemorrhage,8 were complicated with pancreaticfistula.About 6.7% to 25.0% of successfully treated patients had rehemorrhage.[10,11,14,15,25-29]This occurred in 17.8% of our patients.It is difficult to control rehemorrhage,especially in those with repeated rebleeding.Repeated angiography is usually effective in the diagnosis and treatment.In those with lethal massive rehemorrhage,however,rehemorrhage with severe pancreaticfistula or intra-abdominal abscess,there is no satisfied treatment.In our series,rehemorrhage was not predictable and 9 of our patients died of rehemorrhage.Once the bleeding was controlled,vigorous treatment of pancreaticfistula and intra-abdominal abscess is the most effective way to prevent rehemorrhage.
The main cause of mortality in our patients was shock-induced MOF,which accounted for 36.8%(7/19) of overall PPH-related deaths.There were two factors for hemorrhagic shock:one was delayed control of hemorrhage due to unconfirmed diagnosis,and the other was the sudden onset of massive bleeding.Physicians should pay attention to any sign of hemorrhage and make the early diagnosis and treatment.
In conclusion,careful and continuing observation of hemorrhagic signs,especially within the first 24 hours after PD or when the patient has pancreaticfistula or intra-abdominal abscess,is recommended after PD and a prompt treatment is essential once suspected.Although endoscopy and angiography are currently the standard of care for initial management of PPH,surgical approach is still not replaceable.Prevention of hemorrhagic shock and rehemorrhage is the key to preclude the mortality of PPH.
Acknowledgements:The authors would like to thank Yu-Quan Feng,Xiao-Qiang Huang,Wen-Zhi Zhang,Wan-Qing Gu,Rong Liu,Kai Jiang,Xian-Jie Shi,and all other specialists in the Institute of Hepatobiliary Surgery of Chinese PLA General Hospital for their wonderful work over the years.We are also grateful to Yan-Sheng Wang for her help in data collection.
Contributors:HZQ proposed the study.FJ performed research,wrote the first draft and analyzed the data.All authors contributed to the design and interpretation of the study and to further drafts.HZQ is the guarantor.
Funding:None.
Ethical approval:Not needed.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Yeo CJ,Cameron JL,Sohn TA,Lillemoe KD,Pitt HA,Talamini MA,et al.Six hundredfifty consecutive pancreaticoduodenectomies in the 1990s:pathology,complications,and outcomes.Ann Surg 1997;226:248-260.
2 Miedema BW,Sarr MG,van Heerden JA,Nagorney DM,McIlrath DC,Ilstrup D.Complications following pancreaticoduodenectomy.Current management.Arch Surg 1992;127:945-950.
3 Balcom JH 4th,Rattner DW,Warshaw AL,Chang Y,Fernandez-del Castillo C.Ten-year experience with 733 pancreatic resections:changing indications,older patients,and decreasing length of hospitalization.Arch Surg 2001;136:391-398.
4 Yekebas EF,Wolfram L,Cataldegirmen G,Habermann CR,Bogoevski D,Koenig AM,et al.Postpancreatectomy hemorrhage:diagnosis and treatment:an analysis in 1669 consecutive pancreatic resections.Ann Surg 2007;246:269-280.
5 Turrini O,Moutardier V,Guiramand J,Lelong B,Bories E,Sannini A,et al.Hemorrhage after duodenopancreatectomy:impact of neoadjuvant radiochemotherapy and experience with sentinel bleeding.World J Surg 2005;29:212-216.
6 Wei HK,Wang SE,Shyr YM,Tseng HS,Tsai WC,Chen TH,et al.Risk factors for post-pancreaticoduodenectomy bleeding and finding an innovative approach to treatment.Dig Surg 2009;26:297-305.
7 Tien YW,Lee PH,Yang CY,Ho MC,Chiu YF.Risk factors of massive bleeding related to pancreatic leak after pancreaticoduodenectomy.J Am Coll Surg 2005;201:554-559.
8 Rumstadt B,Schwab M,Korth P,Samman M,Trede M.Hemorrhage after pancreatoduodenectomy.Ann Surg 1998;227:236-241.
9 Yoon YS,Kim SW,Her KH,Park YC,Ahn YJ,Jang JY,et al.Management of postoperative hemorrhage after pancreatoduodenectomy.Hepatogastroenterology 2003;50:2208-2212.
10 Choi SH,Moon HJ,Heo JS,Joh JW,Kim YI.Delayed hemorrhage after pancreaticoduodenectomy.J Am Coll Surg 2004;199:186-191.
11 Balachandran P,Sikora SS,Raghavendra Rao RV,Kumar A,Saxena R,Kapoor VK.Haemorrhagic complications of pancreaticoduodenectomy.ANZ J Surg 2004;74:945-950.
12 Makowiec F,Riediger H,Euringer W,Uhl M,Hopt UT,Adam U.Management of delayed visceral arterial bleeding after pancreatic head resection.J Gastrointest Surg 2005;9:1293-1299.
13 Koukoutsis I,Bellagamba R,Morris-Stiff G,Wickremesekera S,Coldham C,Wigmore SJ,et al.Haemorrhage following pancreaticoduodenectomy:risk factors and the importance of sentinel bleed.Dig Surg 2006;23:224-228.
14 Blanc T,Cortes A,Goere D,Sibert A,Pessaux P,Belghiti J,et al.Hemorrhage after pancreaticoduodenectomy:when is surgery still indicated? Am J Surg 2007;194:3-9.
15 Liu C,Qiu YH,Luo XJ,Yi B,Jiang XQ,Tan WF,et al.Treatment of massive pancreaticojejunal anastomotic hemorrhage after pancreatoduodenectomy.World J Gastroenterol 2009;15:1625-1629.
16 Mañas-Gómez MJ,Rodríguez-Revuelto R,Balsells-Valls J,Olsina-Kissler JJ,Caralt-Barba M,Pérez-Lafuente M,et al.Post-pancreaticoduodenectomy hemorrhage.Incidence,diagnosis,and treatment.World J Surg 2011;35:2543-2548.
17 Wente MN,Veit JA,Bassi C,Dervenis C,Fingerhut A,Gouma DJ,et al.Postpancreatectomy hemorrhage (PPH):an International Study Group of Pancreatic Surgery (ISGPS)definition.Surgery 2007;142:20-25.
18 Trede M,Schwall G.The complications of pancreatectomy.Ann Surg 1988;207:39-47.
19 Ellison EC.Evidence-based management of hemorrhage after pancreaticoduodenectomy.Am J Surg 2007;194:10-12.
20 Jagad RB,Koshariya M,Kawamoto J,Chude GS,Neeraj RV,Lygidakis NJ.Postoperative hemorrhage after major pancreatobiliary surgery:an update.Hepatogastroenterology 2008;55:729-737.
21 Bassi C,Dervenis C,Butturini G,Fingerhut A,Yeo C,Izbicki J,et al.Postoperative pancreaticfistula:an international study group (ISGPF) definition.Surgery 2005;138:8-13.
22 Kawai M,Tani M,Hirono S,Ina S,Miyazawa M,Yamaue H.How do we predict the clinically relevant pancreaticfistula after pancreaticoduodenectomy?--an analysis in 244 consecutive patients.World J Surg 2009;33:2670-2678.
23 Bassi C,Falconi M,Molinari E,Mantovani W,Butturini G,Gumbs AA,et al.Duct-to-mucosa versus end-to-side pancreaticojejunostomy reconstruction after pancreaticoduodenectomy:results of a prospective randomized trial.Surgery 2003;134:766-771.
24 Berger AC,Howard TJ,Kennedy EP,Sauter PK,Bower-Cherry M,Dutkevitch S,et al.Does type of pancreaticojejunostomy after pancreaticoduodenectomy decrease rate of pancreaticfistula? A randomized,prospective,dual-institution trial.J Am Coll Surg 2009;208:738-749.
25 Tien YW,Wu YM,Liu KL,Ho CM,Lee PH.Angiographyis indicated for every sentinel bleed after pancreaticoduodenectomy.Ann Surg Oncol 2008;15:1855- 1861.
26 Heiss P,Bachthaler M,Hamer OW,Piso P,Herold T,Schlitt HJ,et al.Delayed visceral arterial hemorrhage following Whipple's procedure:minimally invasive treatment with covered stents.Ann Surg Oncol 2008;15:824-832.
27 Limongelli P,Khorsandi SE,Pai M,Jackson JE,Tait P,Tierris J,et al.Management of delayed postoperative hemorrhage after pancreaticoduodenectomy:a meta-analysis.Arch Surg 2008;143:1001-1007.
28 Fujii Y,Shimada H,Endo I,Yoshida K,Matsuo K,Takeda K,et al.Management of massive arterial hemorrhage after pancreatobiliary surgery:does embolotherapy contribute to successful outcome? J Gastrointest Surg 2007;11:432-438.
29 Okuno A,Miyazaki M,Ito H,Ambiru S,Yoshidome H,Shimizu H,et al.Nonsurgical management of ruptured pseudoaneurysm in patients with hepatobiliary pancreatic diseases.Am J Gastroenterol 2001;96:1067-1071.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Out flow reconstruction with arterial patch in domino liver transplantation:a new technical option
- Th1 cytokine-based immunotherapy for cancer
- Laparoscopic distal pancreatectomy in Italy:a systematic review and meta-analysis
- Laparoscopic liver resection under hemihepatic vascular in flow occlusion using the lowering of hilar plate approach
- Efficacy of ursodeoxycholic acid as an adjuvant treatment to prevent acute cellular rejection after liver transplantation:a meta-analysis of randomized controlled trials
- Long-term results of liver transplantation for over 60 years old patients with hepatitis B virus-related end-stage liver disease
