Prognostic signi fi cance of interim18F-FDG PET/CT SUV reduction associated with Ki67 in patients with diffuse large B-cell lymphoma
2014-04-25SUNYiWen孙一文ZHAOJinHua赵晋华QIAOWenLi乔文礼XINGYan邢岩CHENXiang陈香andSONGJianHua宋建华
SUN Yi-Wen(孙一文),ZHAO Jin-Hua(赵晋华),,QIAO Wen-Li(乔文礼),XING Yan(邢岩),CHEN Xiang(陈香),and SONG Jian-Hua(宋建华)
1Department of Nuclear Medicine,Shanghai First Poeple’s Hospital, Shanghai Jiaotong University,Shanghai 200080,China
Prognostic signi fi cance of interim18F-FDG PET/CT SUV reduction associated with Ki67 in patients with diffuse large B-cell lymphoma
SUN Yi-Wen(孙一文),1ZHAO Jin-Hua(赵晋华),1,∗QIAO Wen-Li(乔文礼),1XING Yan(邢岩),1CHEN Xiang(陈香),1and SONG Jian-Hua(宋建华)1
1Department of Nuclear Medicine,Shanghai First Poeple’s Hospital, Shanghai Jiaotong University,Shanghai 200080,China
To detect the prognostic signif i cance of interim18F-FDG PET/CT SUV(standard uptake value)reduction(ΔSUVmax)associated with Ki67 in patients with diffuse large B cell lymphoma(DLBCL).47 DLBCL patients underwent PET/CT before initiation and after 2–4 cycles of chemotherapy were included.The SUVmaxof the dominant lesions were calculated.Ki67 positive indices were provided by enzyme-labeled immunohistochemistry.SPSS17.0 was used for statistical analysis.ΔSUVmaxof different groups were compared by t test.Receiver-operator characteristic analysis was performed to determine the optimal cutoff values.Kaplan-Meier analyses of PFS(Progression-free survival)were compared using log-rank test.The average of ΔSUVmaxand ΔSUVmax%were 11.53 and 69.10%,respectively.The optimal cutoff values of ΔSUVmaxand ΔSUVmax% were11.45and82.92%,respectively.HigherΔSUVmaxandΔSUVmax%indicatedlongerPFS(p<0.001).The optimal cutoff value of Ki67 was 55%.Ki67≥55%was revealed to be an indicator of shorter PFS(p=0.019). Either ΔSUVmax≤11.45 or Ki67>55%was def i ned as an indicator to poor outcome and scored 1 point.The PFS rate was 100%in patients scored 0 point,yet 0%in patients scored 2 points.PFS tended to be shorter along with the score getting higher(p=0.006).ΔSUVmaxand Ki67 positive index were both of signif i cance in DLBCL prognosis.The prognostic value may be conf i rmed when ΔSUVmaxwas accordant with Ki67.
Diffuse large B cell lymphoma,Standard uptake value,Ki67,Prognosis
I.INTRODUCTION
Diffuse Large B-Cell Lymphoma(DLBCL)is a common lymphoid neoplasm in adults,and is an aggressive Non-Hodgkin Lymphoma(NHL).Thanks to the development of chemotherapeutics,especially the invention of Rituximab, and the progression of autologous stem cell transplantation, DLBCL patients now can maintain remission for a relatively long period.
However,problems such as refractory lymphoma and tumor relapse still make trouble in the management of DLBCL. Also,acute and long-term side effects caused by chemotherapeutic agents play a role in patients’death.To solve these problems,risk-adapted therapy is necessary,the basis of which is assessing prognosis as early as possible.
18F-FDG PET/CT is a metabolic imaging technique refl ecting glucose metabolism.The roles of PET/CT in staging,response assessment,prognosis and follow-up of DLBCL have been demonstrated and brought into guidelines of NHL for years[1],and FDG PET after the therapy proved to be of determinate value for prognosis.However,to do early assessment,PET/CT scans should be performed at earlier stages of the disease treatment,such as after 2 or 4 cycles(interim)of chemotherapy.
Effects were made in detecting an appropriate criterion for interim PET/CT scan.Yet the visual analysis was regarded as not reliable enough by several groups[2,3],and the semiquantitative analysis based on standard uptake value(SUV)was thought to be capable of improving the prognostic accuracy[4],especially the SUV reduction analysis[2,5].
Ki67 is a nuclear antigen expressing in cell generation cycle,and is absent in resting phase cells.It is a dependable parameter for measuring tumor cell proliferation index.High Ki67 positive index was demonstrated to be an indicator of poor outcome[6–9].
As SUV reduction ref l ects the changes of glucose metabolism after therapy,and Ki67 reports tumor cell proliferation index,an integration of them includes information of both aspects.This study is aimed at detecting the prognostic signif i cance of interim18F-FDG PET/CT SUV reduction associated with Ki67 in DLBCL patients.
II.MATERIALS AND METHODS
A.Patients
Forty-seven pathologically conf i rmed DLBCL patients who underwent PET/CT scan from July 2007 to June 2011 were included.Any patients of past tumor history were excluded.All patients accepted f i rst-line chemotherapeutic strategy(CHOP,R-CHOP,or CHOPE)after diagnosis.The follow-up duration ranged from 14–52 months(median 34 months),and the follow-up rate was 95.7%(45/47).The clinical characteristics of the patients are summarized in Table 1.

TABLE 1.Patient Characteristics(n=47)
B.18F-FDG PET/CT
All the patients were scanned on Discovery STE16 PET/CT(GE).Radiochemical purity(>95%)of the FDG and all other specif i cations,met the quality requirements of radiopharmaceuticals.
The patients underwent PET/CT before(initial)and after 2–4 cycles(interim)of chemotherapy.The patients fasted for 6h,and their blood glucose was lower than 7.8mmol/L.The data acquisitions lasted 50–60min after intravenous injection with 0.12–0.15mCi/kg of18F-FDG uptake,which were consisted of 5–7 bed shifts,covering from the upper thigh to the top of the skull.For each bed position except the skull,a 3min emission scan was acquired,and for the bed position of skull,the duration was 5min.The acquisition featured a low dose transmission CT scan(100kV,40mAs,slice thickness: 5mm).
C.SUV-based assessment of18F-FDG uptake
For each PET dataset,the tumor with the most intensive18F-FDG uptake of all foci was carefully identif i ed as the dominant lesion.Regions of interest(ROIs)were drawn around the dominant lesions,and the SUVmaxwere calculated by a computer code on a Xeleris workstation and normalized through body surface area,using Eqs.(1)and(2):

In patients whose lesions disappeared totally after 2–4 cycles of chemotherapy,regions of interest were drawn around the same area in interim PET images as in initial ones. ΔSUVmaxand ΔSUVmax%were calculated as follows:
D.Ki67 positive index
Ki67 positive indices were provided by enzyme-labeled immunohistochemistry.The negative control was PBS,and positive control was given positive section.“Positive result”was def i ned as cell nuclei presenting to be stained for the antigen.For each section,5 high-power f i elds were chosen,200 tumor cells were counted randomly in each f i eld,and the ratio of Ki67 positive tumor cells to 1000 tumor cells was computed.
E.Statistical analysis
SPSS17.0 was used for statistical analysis.PFS was chosen as the endpoint,which was def i ned as the interval from the date of enrollment to the f i rst evidence of progression or relapse or to the date of death from any cause.The data were censored if the patients were alive or free from progression or relapse at the last follow-up.Independent sample t test was used to compare the SUVmaxreduction in patients of different stages,IPIs and follow-up results.Receiver-operator characteristic(ROC)analysis was performed to determine the optimal cutoff values of ΔSUVmax,ΔSUVmax%and Ki67 positive indices for predicting patients’outcome(progression or death vs.free from progression).Survival curves according to SUV-based assessment and Ki67,and the integration of both the variants,were obtained using Kaplan-Meier analysis and were compared using the log-rank test.Signif i cance was obtained when the 2-sidedpvalue was less than 0.05.
III.RESULTS
A.Patients outcome
During the follow up,19(42.2%)of the 45 cases were free from progression.The remaining 26 cases were found to take progression with a median delay of 10.0 months.
B.Prognostic signif i cance ofΔSUVmaxandΔSUVmax%
Before therapy,the SUVmaxwas 18.16±6.54,and it decreased to 5.20±4.89 after 2–4 cycles of chemotherapy.The averaged ΔSUVmaxand ΔSUVmax%were 11.53±5.53 and(69.10±27.90)%,respectively.The ΔSUVmaxand ΔSUVmax%of different groups are given in Table 2. The patients suffered from high IPI and progression during the follow-up showed signif i cantly low ΔSUVmaxand ΔSUVmax%(0.001≤p≤0.008).The ΔSUVmax%was also signif i cantly low in stage IV patients.The ΔSUVmaxtended to be low in stage IV patients,though the difference was no signif i cant.
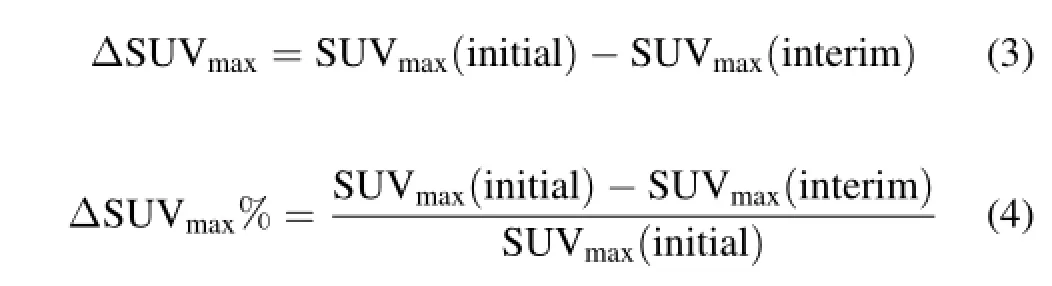
According to ROC analysis,the optimal cutoff values of ΔSUVmaxand ΔSUVmax%were 11.45 and 82.92%for PFS prediction,respectively(Fig.1).The accuracies were84.4%(area under the curve,0.842)and 80%(area under the curve,0.889),respectively.The PFS rate of different groups and the predictive value using ΔSUVmaxand ΔSUVmax%are given in Table 3.

TABLE 2.ΔSUVmaxand ΔSUVmax%of different groups
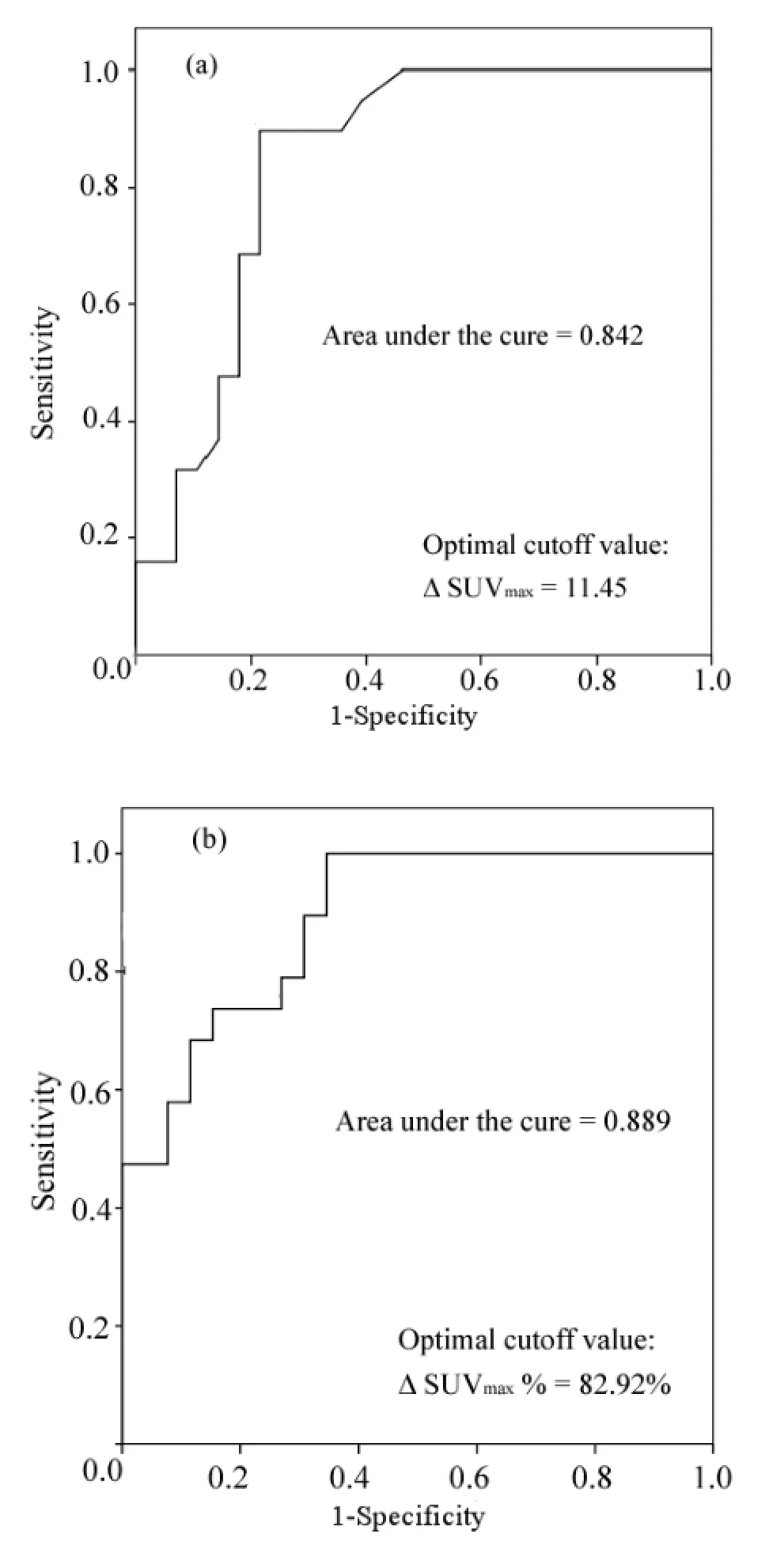
Fig.1.ROC analysis of ΔSUVmax(a)and ΔSUVmax%(b)for PFS prediction.

TABLE 3.Predictive value based on ΔSUVmaxand ΔSUVmax%

TABLE 4.PFS estimates
Kaplan-MeierestimatesofPFSaccordingtoΔSUVmaxand ΔSUVmax%are shown in Fig.2,which reveals that the patients with higher ΔSUVmaxand ΔSUVmax%are of longer PFS.The PFS data are given in Table 4.
C.Prognostic signif i cance of Ki67 positive index
With a 55%optimal cutoff value of Ki67 positive index calculated using ROC curve(Fig.3),the PFSs are given in Table 4.The accuracy of Ki67 for predicting 2-year PFS is 80%(PPV=77.8%,andNPV=81.2%).Kaplan-Meierestimates based on Ki67 are shown in Fig.4,which indicates that Ki67>55%can be an indicator to shorter PFS(p=0.019).
D.Prognostic signif i cance ofΔSUVmaxassociated with Ki67

Fig.2.(Color online)Kaplan-Meier estimates of PFS according to ΔSUVmax(a)and ΔSUVmax%(b).Patients with ΔSUVmax>11.45 and ΔSUVmax>82.92%were revealed to be of longer PFS.
Both the ΔSUVmaxand Ki67 data were collected from 20 patients.From the results above,the prognostic value of both ΔSUVmaxand Ki67 for PFS were conf i rmed.Assuming an integrative score system as ΔSUVmax≤11.45 and Ki67>55% being indicators to poor outcome(“negative”for predicting PFS)with a score of 1 point,the scores and outcomes are given in Table 5.The PFS is 100%(5/5)in patients scored 0 point(“double positive”),but 0%(0/7)in patients scored 2 points(“double negative”).That means,for predicting PFS, the PPV of 0 score group and the NPV of 2 score group are both as high as 100%.The accordance of ΔSUVmaxand Ki67 may conf i rm the prediction of patients’outcome.PFS estimates based on the integrative score system using Kaplan-Meier methods are shown in Fig 5.
Fig.3.ROC curve analysis of Ki67 positive index for PFS predicting,at the optimal cutoff value of 55%,sensitivity of 86.7%and specif i city of 70%,with the accuracy being 80%.

Fig.4.(Color online)Kaplan-Meier estimates of PFS based on Ki67 with Ki67>55%being an indicator of shorter PFS(χ2=5.488,p=0.019).
IV.DISCUSSIONS
Since 2007 when PET/CT was incorporated into the response evaluation criteria of NHL by the International Harmonization Project(IHP)in 2007[1],the signif i cance of PET/CT in NHL has been demonstrated.In a systematic review by Terasawa Tet al.[10]on 19 studies that included 474 patients of Hodgkin disease and 254 NHL patients,the signif i cance of PET/CT in identifying necrosis and residualtumors after chemotherapy was conf i rmed.However,this is not enough for NHL management.In order to maintain remission and minimize side effect,it is necessary to assess the outcomes as early as possible.International prognostic index, which has been used for years,is a prognostic factor based on population.However,metabolic imaging such as PET/CT is of potential capacity for individual prognosis.In a study including 8 aggressive NHL patients,SUVmaxdecreased by 60%one week after the f i rst dose of chemotherapy[11].The potency of PET/CT for early prognosis was conf i rmed by this result.Nowadays,early(after 2 cycles of chemotherapy)and interim(after 4 cycles)PET/CT assessments are of concern in NHL[5,12].
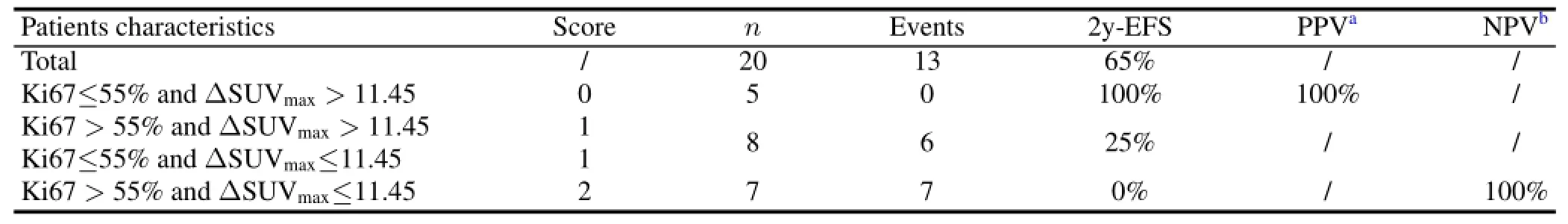
TABLE 5.Scores of ΔSUVmaxassociated with Ki67 positive index
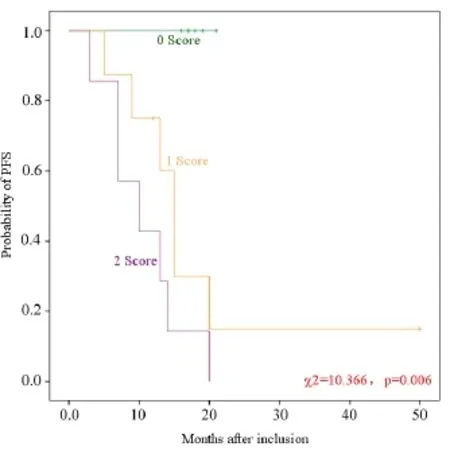
Fig.5.(Color online)Kaplan-Meier estimates of PFS based on the integrative score system,revealing that the PFS tended to be shorter along with the scores getting higher(χ2=10.366,p=0.006).
Since the accuracy of early or interim PET/CT for assessing patients’outcome was not high enough by just visual analysis according to various criteria[2,3,13],it is believed that the prognostic accuracy can be improved through SUV analysis[4].SUV is a semi quantitative parameter measured in daily PET/CT scan,which has advantages such as noninvasive,easy to calculate and wide application.However, controversy exists because of its susceptibility to various factors.It is necessary to do something to minimize the inf l uencing factors.In this study,all the acquisitions were performed on the same machine in the same institution,ensuring no infl uenceofthemachinetypeiscaused.Scansweredone50–60 minutes after the tracer injection,which is considered as the duration required for the FDG uptake to reach a plateau,so the in fl uence caused by imaging delay was minimized.And in order to decrease the partial-volume effect,SUVmaxwas chosen instead of SUVmean.By controlling imaging conditions,SUVmaxwas repeatable[14].
However,SUV calculations are affected by a number of factors,which cannot be avoided totally.Therefore,SUV reductionbasedonthesamemachine,thesameacquisitionconditions and the same method of normalization might be more reliable.In studies including 92 DLBCL patients,the optimal cutoff values of SUVmaxreduction after 2 and 4 cycles of chemotherapy were 65.7%and 72.9%,respectively[5,12], with PPVs of 81.3%and 70.6%,and NPVs of 76.1%and 79.4%,respectively.These studies also pointed out that the prognostic value of SUVmaxreduction analysis showed no signi fi cant difference after 2 cycles and after 4 cycles of therapy,through visual analysis did show a higher prognostic value after 4 cycles than that after 2 cycles.Similarly,the present study con fi rmed the signi fi cance of SUVmaxreduction in DLBCL patients’prognosis,but due to the limit of patient number,the“interim PET/CT”was not restricted to be performed after 4 cycles(4 after 2 cycles and 1 after 3 cycles), which was a heterogeneity in this study.
Ki67 positive index is a marker of tumor cell proliferation,and high Ki67 means a risk factor in various malignant tumors[15–17],including lymphoma[6–9].In a study including 58 DLBCL patients who accepted R-CHOP chemotherapy,Ki67>80%was an indicator of shorter PFS and OS[18].Shouet al.[19]revealed a positive correlation between Ki67 and FDG uptake in NHL, fi guring out that the SUVaveof the LCL(large cell lymphoma)group was signi ficantlyhigherthanthatoftheSCL(smallcelllymphoma)with relatively little overlap between the groups.
Several groups suggested that by integrating SUV analysis with other clinical risk factors,the prognostic value might be improved.In Ref.[20],a parameter named“SIMaxSUV”was de fi ned as SUVmaxmultiplied by the maximal diameter of the dominant lesion,and used as an independent prognostic factor for PFS.In Ref.[21],scores counted by integration of SUVmaxreduction,age-adjusted IPI and molecular subtype of DLBCL used as signi fi cance in predicting OS.
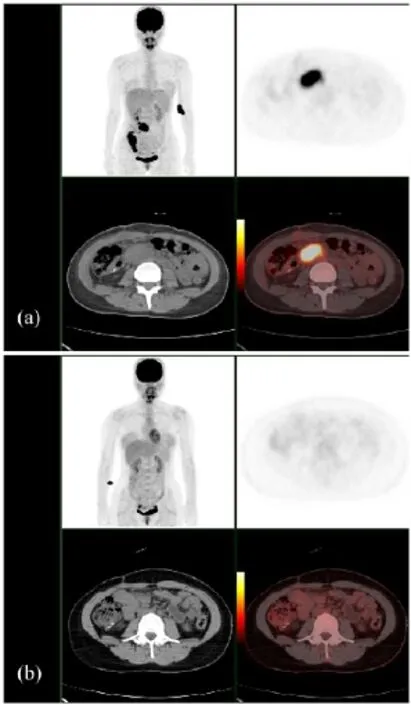
Fig.6.(Color online)PET/CT images of a 29 years-old female, DLBCL stage IV,Ki67 of 50%.The initial scan found mesenteric lymph nodes and right colon involvement,SUVmaxwas 21.9(a),interim PET/CT found no apparent malignant lesion and SUVmaxwas 2.0(b),ΔSUVmaxand ΔSUVmax%were 19.9 and 90.9%,respectively.Integrative score was 0.Although the age-adjusted IPI was high,no symptom of progression or relapse was found during the follow-up of 26 months.
In FDG PET/CT,the false positive results caused by infl ammatory response after therapy can be the most important factor affecting the accuracy of prognosis.18F-FLT,which is an analogue of thymine,can ref l ect the cell proliferation level,and is conf i rmed to be a negative predictor of response correlating with the IPI scores[22].FLT is known to be able to decrease the false positive results caused by in fl ammatory response,but it is not yet applied routinely in clinic.Fortunately,Ki67,which is widely used in clinical practice to refl ect tumor proliferation,is also of signi fi cance for prognosis, as mentioned above.
An attempt was made in this study to evaluate the prognostic signi fi cance of the integration of interim SUV reduction and Ki67 positive index.However,no signi fi cant difference was found between the prognostic values of ΔSUVmaxand ΔSUVmax%,withpvalues of 0.970 and 0.318,respectively, comparing with their PPVs and NPVs through two dimensional cross tables.
It was observed that the PPV of 0-score patients and NPV of 2-score patients were both as high as 100%.This score system integrated two important aspects of tumor biological behavior,glucose metabolism and tumor cell proliferation, which might be the feasibility for improving the prognostic capacity.Although the sample size was somewhat small,the accordance of these two parameters seemed to con fi rm the prognosis,especially in the 0-score group(Fig.6),implying that low Ki67 could be helpful in selecting a subset of patients,for whom a high reduce of FDG uptake means a very good prognosis.
However,limited by the clinical practice,no data about Ki67 reduction was collected,which might be more associated with SUVmaxreduction and more accurate for outcome predicting.On the other hand,potential clinical implications after interim PET/CT scan were not taken into consideration, which might somewhat affect patients’outcomes.Further efforts will be made in expanding the sample size and recording Ki67 after therapy.A perspective study to minimize the variety of SUVs and exclude the potential impact derived from therapeutic alteration,shall be devised.
V.CONCLUSION
In summary,ΔSUVmaxand Ki67 positive index were both of signif i cance in DLBCL prognosis.The prognostic accuracy may be conf i rmed when ΔSUVmaxwas in accordance with Ki67,especially in selecting patients with pretty good outcomes.Further perspective study with large sample shall be contributing.
[1]Cheson B,Pf i stner B,Juweid M,et al.J Clin Oncol,2007,25: 579–586.
[2]Pregno P,Chiappella A,Bell`o M,et al.Blood,2012,119: 2066–2073.
[3]Cox M C,Ambrogi V,Lanni Vet al.Leukemia Lymphoma, 2012,53:263–269.
[4]Casasnovas R O,Meignan M,Berriolo-Riedinger A,et al. Blood,2011,118:37–43.
[5]Lin C,Itti E,Haioun C,et al.J Nucl Med,2007,48:1626–1632.
[6]Broyde A,Boycov O,Strenov Y,et al.Am J Hematol,2009,84:338–343.
[7]Bryant R J,Banks P M,O’Malley D P,et al.Histopathology, 2006,48:505–515.
[8]Szczuraszek K,Mazur G,Jelen M,et al.Anticancer Res,2008,28:1113–1118.
[9]Kim S J,Kim B S,Choi C W,et al.Ann Oncol,2007,18: 1382–1387.
[10]Terasawa T,Nihashi T,Hotta T,et al.J Nucl Med,2008,49: 13–21.
[11]Wu X,Dastidar P,Pertovaara H,et al.Mol Imaging Biol,2011,13:785–792.
[12]Itti E,Lin C,Dupuis J,et al.J Nucl Med,2009,50:527–533.
[13]Itti E,Juweid M E,Haioun C,et al.J Nucl Med,2010,51: 1857–1862.
[14]Nahmias C and Wahl L M.J Nucl Med,2008,49:1804–1808.
[15]Han B,Lin S,Yu L J,et al.Nucl Med Commun,2009,30: 831–837.
[16]Ueda S,Tsuda H,Saeki T,et al.Breast Cancer,2011,18:299–308.
[17]Tang B,Malysz J,Douglas-Nikitin V,et al.Mol Imaging Biol, 2009,11:296–302.
[18]Gaudio F,Giordano A,Perrone T,et al.Acta Haematol,2011,126:44–51.
[19]Shou Y,Lu J,Chen T,et al.J Cancer Res Ther,2012,8:96–102.
[20]Nguyen X C,Lee W W,Amin A M,et al.Nucl Med Mol Imaging,2010,44:39–44.
[21]Lanic H,Mareschal S,Mechken F,et al.Leukemia Lymphoma, 2012,53:34–42.
[22]Herrmann K,Buck A K,Schuster T,et al.J Nucl Med,2011,52:690–696.
10.13538/j.1001-8042/nst.25.020304
(Received May 13,2013;accepted in revised form September 5,2013;published online April 20,2014)
∗Corresponding author,zjh1963@gmail.com
猜你喜欢
杂志排行
Nuclear Science and Techniques的其它文章
- A hybrid voxel sampling method for constructing Rad-HUMAN phantom∗
- Measurement of keffwith an improved neutron source multiplication method based on numerical analysis∗
- Simulation of neutron diffusion and transient analysis of MSR∗
- Ordered water monolayer on ionic model substrates studied by molecular dynamics simulations∗
- A method for determination of the s orbital component of12Be ground state∗
- Demonstration of Pm-147 GaN betavoltaic cells