Cardiac arrest - cardiopulmonary resuscitation
2014-03-21BasriLenjaniNehatBaftiuKelmendPallaskaKadirHyseniNjaziGashiNexhbedinKaremaniIlazBunjakuTaxhidinZaimiArianitJakupiBesnikElshani
Basri Lenjani, Nehat Baftiu, Kelmend Pallaska, Kadir Hyseni, Njazi Gashi, Nexhbedin Karemani, Ilaz Bunjaku, Taxhidin Zaimi, Arianit Jakupi, Besnik Elshani
1Emergency Clinic, University Clinical Centre of Kosovo, Pristina 10000, Republic of Kosovo
2Anesthesiology Clinics, University Clinical Centre of Kosovo, Pristina 10000, Republic of Kosovo
3Radiology Clinic, University Clinical Centre of Kosovo, Pristina 10000, Republic of Kosovo
Cardiac arrest - cardiopulmonary resuscitation
Basri Lenjani1*, Nehat Baftiu1, Kelmend Pallaska1, Kadir Hyseni2, Njazi Gashi2, Nexhbedin Karemani2, Ilaz Bunjaku3, Taxhidin Zaimi3, Arianit Jakupi3, Besnik Elshani3
1Emergency Clinic, University Clinical Centre of Kosovo, Pristina 10000, Republic of Kosovo
2Anesthesiology Clinics, University Clinical Centre of Kosovo, Pristina 10000, Republic of Kosovo
3Radiology Clinic, University Clinical Centre of Kosovo, Pristina 10000, Republic of Kosovo
Objective: To investigate application of cardiopulmonary resuscitation (CPR) measures within the golden minutes in Europe. Methods: The material was taken from the University Clinical Center of Kosovo - Emergency Centre in Pristina, during the two (2) year period (2010-2011). The collected date belong to the patients with cardiac arrest have been recorded in the patients' log book protocol at the emergency clinic. Results: During the 2010 to 2011 in the emergency center of the CUCK in Pristina have been treated a total of 269 patients with cardiac arrest, of whom 159 or 59.1% have been treated in 2010, and 110 patients or 40.9% in 2011. Of the 269 patients treated in the emergency centre, 93 or 34.6% have exited lethally in the emergency centre, and 176 or 65.4% have been transferred to other clinics. In the total number of patients with cardiac arrest, males have dominated with 186 cases, or 69.1%. The average age of patients included in the survey was 56.7 year old SD ± 16.0 years. Of the 269 patients with cardiac arrest, defibrillation has been applied for 93 or 34.6% of patients. In the outpatient settings defibrillation has been applied for 3 or 3.2% of patients. Patients were defibrillated with application of one to four shocks. Of 27 cases with who have survived cardiac arrest, none of them have suffered cardiac arrest at home, 3 or 11.1% of them have suffered cardiac arrest on the street, and 24 or 88.9% of them have suffered cardiac arrest in the hospital. 5 out of 27 patients survived have ended with neurological impairment. Cardiac arrest cases were present during all days of the week, but frequently most reported cases have been on Monday with 32.0% of cases, and on Friday with 24.5% of cases.
Conclusions: All survivors from cardiac arrest have received appropriate medical assistance within 10 min from attack, which implies that if cardiac arrest occurs near an institution health care (with an opportunity to provide the emergent health care) the rate of survival is higher.
ARTICLE INFO
Article history:
Received 20 August 2013
Received in revised form 19 September 2013
Accepted 19 October 2013
Available online 20 March 2014
Cardiac arrest
1. Introduction
Cardiac arrest is the cessation of cardiac mechanical activity, confirmed by the lack of pulse, respiration, and loss of consciousness. Most of the cases with cardiac arrests in the hospital are originated from the heart. There is not, however, over-estimated the arrest report originated from, if it is not confirmed by autopsy. Each year about 500 000 people in Europe are victims of cardiac arrest. CPR applied by laymen survival rate increases to 2-3 times, if applied in outpatient settings. The implementation of CPR measures within golden minutes in Europe may save lives 100 000 persons per year. In Europe every 45 s happen a cardiac arrest. Quick rescutitation and early defibrillation (within 1-2 min) can increase survival > 60%. In Kosovo during a year we have 4 000-5 000 every year in an hour a cardiac arrest occurs within 24 h 13.7 cases are presented. In Kosovo every 1:51 min a cardiac arrest occurs. If CPR is applied within minutes golden, the survival of victims will reach 34%, compared with the 2005 CPR guidelines, which survival amounts to 18% of victims. These data come from the new guidelines from the “American Heart Association 2010”Under this amended standard procedures by ABC (Airways, Breathing-Compressions) apply and vary actions,’’ ABCto “CAB” (Compressions-Airways-Breathing). Savior who are trained and ready to make the move, cardiac massage can be combined with artificial respiration, in the ratio of 30 pressures in the chest and two life-breath. Basic life support - basic life support (BLS) is the fundamental basis for life - saving cardiac arrest victims after as to (illnesses, injuries and poisonings) BLS fundamental aspects include: Early recognition of sudden cardiac arrest, activation of the emergency response system, early CPR, rapid defibrillation (AED).
Two main steps of saving lives: Medical Emergency 112 Call, press quickly strong in the center of the chest. Quality of CPR - BLS - in outpatient and inpatient settings to victims of cardiac arrest is often weak in most cases, and should develop methods to improve the quality of CPR, particularly in Kosovo conditions. Advanced cardiac life support (ACLS) - ACLS interventions intended to prevent cardiac arrest in particular by include: managing the respiration, ventilation support, handling bradyrhythmia and tachyarrythmia. Advanced cardiac life support (ACLS), which administered medications, cardiac monitoring and other technical-medical.
The main purpose of this paper to reduce the incidence, longevity and mortality of persons from cardiac arrest in the street, at home and in hospital environments for the implementation of early fast intervention of CPR to save people’s lives with life threatening. The implementation of basic life support (BLS) and learn how to work advanced cardiac life support (ALCS) is the fundamental purpose of saving the lives of victims with cardiac arrest.
2. Materials and methods
The material is taken from the University Clinical Center of Kosovo - Emergency Clinic in Prishtina on two-year period 2010-2011. The data were derived from the protocol of the emergency clinic patients with cardiac arrest patients.
There are investigated only patients with cardiac arrest origined cardiac. Purpose is realized on the basis of: the anamnesis, vital status parameters, objective examination results, diagnostic research-laboratory and radiology, statistical parameters, the index structure, and the arithmetic average and standard deviation.
Statistical tests: χ2-test and t-tests. Test verification is made for 95% confidence level and 99%, respectively P<0.01 and P<0.05.
3. Results
In the UCC emergency clinic in Prishtina during 2010-2011 were treated 269 patients with cardiac arrest from which 159 or 59.1% were treated in 2010 while 110 or 40.9% in 2011 (Table 1).
The average age of the patients included in the survey was 56.7 years (SD±16.0 years), the youngest patient was under 1 year and the oldest 92 years.
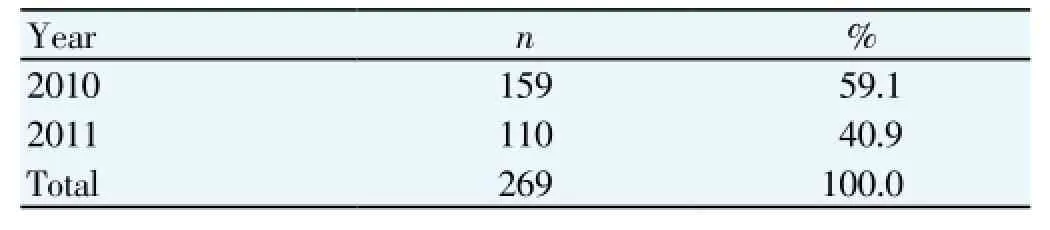
Table 1. Number of patients with cardiac arrest in years.

Table 2. Parameters age of the patients by gender.
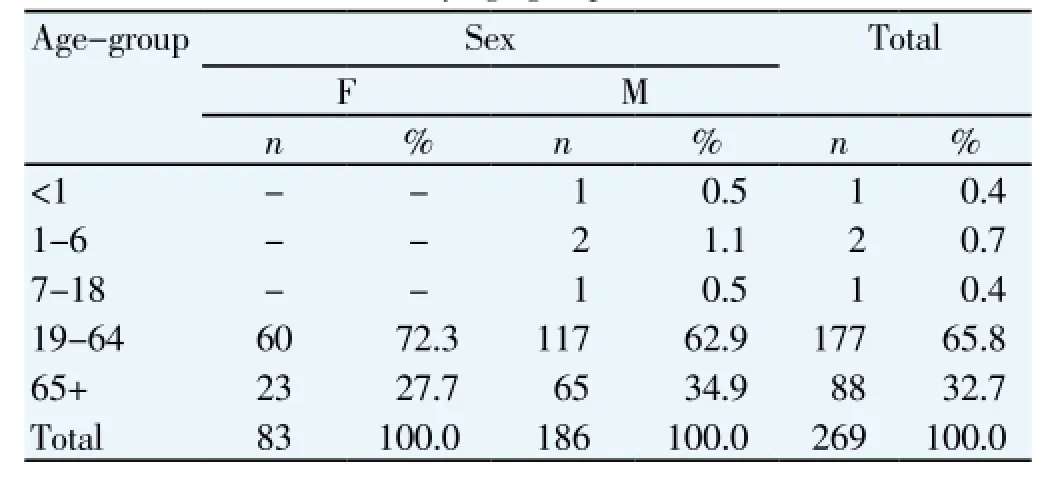
Table 3. Patients with cardiac arrest by age group and sex.
The average age of female patients included in the survey was 55.2 years (SD±14.6 years), the youngest patient was 20 years and the oldest 92 years. The average age of male patients included in the survey was 57.3 years (SD±16.6 years), the youngest patient was under 1 year and the oldest 87 years. T-test averages have not earned the distinction with important statistically significant between the average age by gender (t = 0.99, P>0.05) (Table 3).
As shown in Table 5 we had only one case or 0.4% children less than one year, two cases or 0.7% 1-6 years, 1 case or 0.4% of the age group 7-18 years, 177 cases or 65.8% of 19-64 years age group and 88 cases or 32.7% were 65 or more years. Children with cardiac arrest have been only males, while patient females were adult 19-64 years 72.3% and 65or more years 23 or 27.7%.

Table 4. Pathophysilogy forms of presentation in early ECG CPR procedures.
In early cardiopulmonary resuscitation procedures we had 20 patients or 7.4% of all patients with ventricular tachycardia, 39 or 14.5% with ventricular fibrillation, 193 or 71.7% of Asystole and 17 or 6.3% with no pulse electrical activity (electromechanical dissociation) (Table 6). At the end of the CPR procedures we had 26 patients or 9.7% of all patients with ventricular tachycardia, 34 or 12.6% with ventricular fibrillation, 168 or 62.5% of Asystole, 14 or 5.2% of electrical activity without pulse and 27 or 10.0% the normal rythm (Table 7). Of 269 patients with cardiac arrest defribillation is applied to 93 or 34.6% (Figure 5). In outpatien settings defribillation is made to three or 3.2% of patients (Table 4).
Cardiopulmunary resuscitation of 243 patients or 90.3% is applied in hospital environments, to 3 or 1.1% is applied in outpatient settings and 37 or 13.8% is applied cardiopulmonary resusciation (Table 5).
The defribilliated patiens are applied from a shock stroke to four shock strokes. A shock stroke is applied to 20 patients or 21.5%, two shock strokes to 38 or 40.9%, three shock strokes to 22 or 23.7% and four shock strokes to 13 or 14.0% (Table 6).

Table 5. The number of patients defibrillated in outpatient settings and hospital environments.
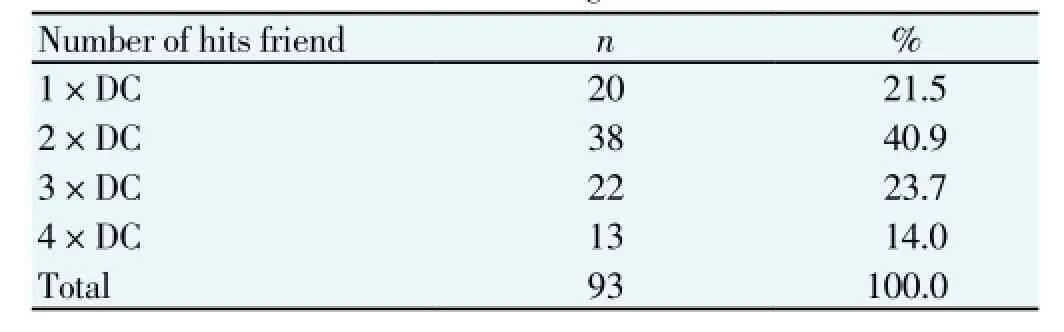
Table 6. Defibrilliation number of actions during CPR measures.
Cardiopulmonary resuscitation of 243 patients or 90.3% is applied in hospital environments, to 3 or 1.1% is applied in outpatient settings and 37 or 13.8% is applied cardiopulmonary resusciation (Table 7). In our clinical material 242 or 90.0% of the patients were endotracheal Intubation. The four patients or 1.5% endotracheal intubation is made in outpatient settings, the 238 or 88.5% in hospital environment (from 269 193 patients with cardiac arrest or 71.7% came in emergency wthout life-signs, and 76 or 28.3% of patients had pupil-dilated less than 4 mm.

Table 7. The number of patients in whom CPR measures are implemented.
At the end of treatment in UCC 242 patients or 90.0% are fatal, whereas only 27 patients or 10.0% survive. Those survivors of cardiac arrest have received adequate medical aid within 10 min after the attack. Out of the total number 3 or 11.1% were treated within the first and second minutes after the attack, 21 or 77.8% in the third minute and the fourth and three others from the fifth minute to ten minutes after the attack.

Table 8. The number of survivors of cardiac arrest at home sick, roads and hospital.

Table 9. Cardiac arrest occurred by days of the week.
There were no survivors when medical aid is provided later. Of the 27 cases of cardiac arrest survivors none of them had cardiac arrest at home, 3 or 11.1% had cardiac arrest in the street and 24 or 88.9% had cardiac arrest in hospital. Which means that if the cardiac arrest occurs near health institution (ability to give emergency aid) survival rate is higher (Table 8) As shown in Table 8, the 27 survivors 5 or 18.5% have completed neurological damage. Cases with cardiac arrest has had on all days of the week but mostly there was on Monday with 32.0% of cases, then on Friday with 24.5% while other days is similar and ranges from 12.6%on Wednesday, 10.8% on Thursday, 9.7% on Saturday, 9.3% on Tuesday and 8.6% on Sunday (Table 9).
4. Discussion
Cardiac arrest is the leading cause of sudden death. The implementation of CPR measures within the gold minutes in Europe may save lives of 100 000 people in a year. In Helsinki, Finland, 67% of all cardiac arrest with cardiac origin are verified by autopsy. 90% of cardiac arrests occured in Sweden, are cardiac origin, as a result of ischemic heart disease, while 10% are due to heart disease and other diseases, such as valvular or cardiomyopathy. In Kosovo within a year there are 4 000-5 000 every one hour a cardiac arrest occurs and within 24 h occur to 13.7 cases.
In Kosovo every 1:51 min occurs a cardiac arrest. Cardiac arrest in outpatient settings in Kosovo is more common among different age group, with very high mortality results[4]. Women who suffer from cardiac arrest increases about 29% share, the mortality rate in Europe is still high[1,3,4]. Therefore, strict implementation of the new CPR recomandation will significantly help to reduce disability and mortality in Kosovo. Whereas in America and Europe is significantly lower.
In America and Europe disability and mortality from cardiac arrest is lower in comparison with Kosovo. While the developed countries like America, Sweden, Australia, France, Germany etc. economically well developed, have invested in legislation regulating care emergency medical services in outpatient settings and hospital environment.
This has affected the provision of medical services for emergent medical supplies and education and training and education of nurses and doctors as well as population. But in Kosovo emergency medical services are developing and in the future remains to be emergency medical services priority to Ministry of Health and the Government of Kosovo. For this reason emergency medical services to us and in Europe do not generate revenue but to persons escape danger.
Recommendations
Support, advancement and empowerment of the SHEM by the Ministry of Health in three levels of organisation of the health system to support these directions as in: Advancement and empowerment of emergency medical services and hospital environment and outpatient settings. Establishing standards for ambulances For ex SHEM outpatient settings. Establishing long-term policies and strategies for SHEM.
Education and continuous training of staff in emergency outpatient settings and hospital environments. Establishing protocols, algorithms and guide clinic Formation of cardiac medical teams and hospital environment and outpatient settings.
To encourage and develop emergency medical services as an integral part of the unique health system. The goals of the national program models SHEM, which are mandatory to be regulated through legislation and laws to be implemented.
Conflict of interest statement
We declare that we have no conflict of interest
Reference
[1] Hupfl M, Selig HF, Nagele P. Chest-compression-only versus standard cardiopulmonary resuscitation: a meta-analysis. Lancet 2010; 376(9752): 1552-1557.
[2] Berg RA, Hemphill R, Abella BS, Aufderheide TP, Cave DM, Hazinski MF, et al. Part 5: Adult Basic Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S685-S700.
[3] Ogawa T, Akahane M, Koike S, Tanabe S, Mizoguchi T, Imamura T. Outcomes of chest compression only CPR versus conventional CPR conducted by lay people in patients with out of hospital cardiopulmonary arrest witnessed by bystanders: nationwide population based observational study. BMJ 2011; 342: c7106.
[4] Vanden Hoek TL, Morrison LJ, Shuster M, Donnino M, Sinz E, Lavonas EJ, et al. Part 12: cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S819-S851.
[5] Field JM, Hazinski MF, Sayre MR, Chameides L, Schexnayder SM, Hemphill R, et al. Part 1: Executive Summary: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S640-S650.
[6] Sayre MR, O’Connor RE, Atkins DL, Billi JE, Callaway CW, Shuster M, et al. Part 2: evidence evaluation and management of potential or perceived conflicts of interest: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S650-S661.
[7] Morrison LJ, Kierzek G, Diekema DS, Sayre MR, Silvers SM, Idris AH, et al. Part 3: Ethics: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and EmergencyCardiovascular Care. Circulation 2010; 122: S664-S672.
[8] Travers AH, Rea TD, Bobrow BJ, Edelson DP, Berg RA, Sayre MR, et al. Part 4: CPR Overview: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S676-S672.
[9] Berg RA, Hemphill R, Abella BS, Aufderheide TP, Cave DM, Hazinski MF, et al. Part 5: Adult Basic Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S685-S697.
[10] Link MS, Atkins DL, Passman RS, Halperin HR, Samson RA, White RD, et al. Part 6: electrical therapies: automated external defibrillators, defibrillation, cardioversion, and pacing: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S706-S719.
[11] Cave DM, Gazmuri RJ, Otto CW, Nadkarni VM, Cheng A, Brooks SC, et al. Part 7: CPR techniques and devices: 2010 American Heart Association Guidelines for CardiopulmonaryResuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S720-S728.
[12] Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, et al. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S729-S757.
[13] Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, et al. Part 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitationand Emergency Cardiovascular Care. Circulation 2010; 122: S768-S766.
[14] O’Connor RE, Brady W, Brooks SC, Diercks D, Egan J, Ghaemmaghami C, et al. Part 10: acute coronary syndromes: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S787-S807.
[15] Jauch EC, Cucchiara B, Adeoye O, Meurer W, Brice J, Chan YY, et al. Part 11: adult stroke: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S818-S818.
[16] Vanden Hoek TL, Morrison LJ, Shuster M, Donnino M, Sinz E, Lavonas EJ, et al. Part 12: cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S829-S861.
[17] Berg MD, Schexnayder SM, Chameides L, Terry M, Donoghue A, Hickey RW, et al. Part 13: pediatric basic life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S862-S865.
[18] Bhanji F, Mancini ME, Sinz E, Rodgers DL, McNeil MA, Hoadley TA, et al. Part 16: education, implementation, and teams: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S920-S923.
[19] Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, et al. Part 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122(18 Suppl 3): S768-S786.
[20] Vanden Hoek TL, Morrison LJ, Shuster M, Donnino M, Sinz E, Lavonas EJ, et al. Part 12: cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S829-S841.
[21] Mary Fran Hazinski. Highlights of the 2010. American Heart Association Guidelines for CPR and ECC. Texas: American Heart Association; 2010, p. 11-18.
[22] Trinkle RM, Flabouris A. Documenting rapid response system afferent limb failure and associated patient outcomes. Resuscitation 2011; 82: 810-804.
[23] Sandroni C, Cavallaro F. Failure of the afferent limb: a persistent problem in rapid response systems. Resuscitation 2011; 82: 797-798.
[24] Judith Tintinalli. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. Seventh Edition. New York: McGraw-Hill Professional 2011, p. 39-44; 44-49; 76-69.
[25] A New Order for CPR, Spelled C-A-B: American Heart Association Guidelines (Oct. 18, 2010) The American Heart Association is re-arranging the ABCs of cardiopulmonary resuscitation (CPR) in its 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency 2010; 28-77.
[26] Mary Fran Hazinski, Ricardo Samson, Steve Schexnayder. American Heart Association Handbook of Emergency Cardiovascular Care for Healthcare Providers (AHA Handbook of Emergency Cardiovascular Care) 2010; 17-29.
[27] American Heart Association. Highlights of the 2010 American Heart Association Guidelines for CPR and ECC. [Online]. Available form http://static.heart.org/ eccguidelines/pdf/ucm_317350.pdf. [Accessed on Dec. 11, 2010].
[28] An archive University Clinical Centre of Kosovo Emergency Clinic of, Pristina, 2010-2011.
ment heading
10.1016/S2221-6189(14)60007-X
*Corresponding author: Basri Lenjani, MD. University Clinic Clinical Emergency, Center of Kosovo, Pristina, Kosovo.
Tel: +377 44165770
E-mail: basrilenjani@yahoo.com
Emergency center
University clinical centre of Kosovo
杂志排行
Journal of Acute Disease的其它文章
- Acute reaction to erroneous injection of adrenaline to the patients with hyperthyroidism
- Acute hepatitis with observed increased blood phenytoin level: a case study
- The value of C-reactive protein in emergency medicine
- Attitude and perception of junior resident doctors’ regarding antibiotic resistance - A pilot study
- MRSA toxic shock syndrome associated with surgery for left leg fracture and co-morbid compartment syndrome
- Stromal opacity secondary to preservative in dilating drops - A case report and review of literature
