Surgical treatment of hydrocephalus and spinal dysraphism
2014-03-21BesnikElshaniBasriLenjani
Besnik Elshani, Basri Lenjani
Emergency Clinic University Clinical. Center of Kosovo, Prishtina, Kosovo
Surgical treatment of hydrocephalus and spinal dysraphism
Besnik Elshani*, Basri Lenjani
Emergency Clinic University Clinical. Center of Kosovo, Prishtina, Kosovo
Objective: To identify during intrauterine congenital malformations; Surgery to dysraphism and hydrocephalus neurological benefit, the ability to live independently; Forecast possibility of lowering birth rates with congenital malformations. Methods: Epidemiological and congenital malformations of the spinal dysraphism were included in this prospective clinical studyresearch. Its forms were manifested by the appearance of hydrocephalus in Neurosurgical Clinic in Pristina for the period 2010-2012. All cases of spinal dysraphism operated in the Neurosurgery Clinic in Prishtina for the period 2010-2012 were analyzed. Results: In the Neurosurgery Clinic at UCC since 2010 to 2012 are operated total 55 cases of spinal dysraphism; The largest number of operations were recorded in 2011 with 20 operated cases or 36.36%, while smaller in 2010 with 17 operated cases or 30.91%, Number of patients varies by year, with some variations of the graph, where at the beginning of the graph have gradually increased over the years, following the continuous growing and finally landing back with graph; By sex and years, the largest number of cases in male gender with spinal dysraphism were registered in 2012 with 14 cases or 37.8%, while the smallest number in 2010 with 11 cases or 29.7%, Whereas the female gender, number of large backlog of cases was registered in 2011 with 8 cases or 44.4%, while the smallest number in 2012 with 4 cases or 22.2%. Divided by types of spinal dysraphism total were identified: 13 with spinal dysraphism meningocele or 23.6% and 42 spinal dysraphism myelomeningocele or 76.4% of which were male dominance in relation to female sex ratio (M:F = 40:15 occasions), by gender and spinal dysraphism species, the males are identified with many cases, the spinal dysraphism meningocele 8 or 20% and 32 with spinal dysraphism myelomeningocele or 80%, Eksterioizm Shanti where the body rejects foreign body system as the one we had at 1 patient. Conclusions: Shant meningitis due to infection or eventual reduction in immune intervention, was warned to 5 patients; Hematoma bilateral subdural due to excessive absorption of the system is evidenced in 1 patient.
ARTICLE INFO
Article history:
Received 20 August 2013
Received in revised form 19 September 2013
Accepted 19 October 2013
Available online 20 March 2014
Surgical treatment
Hydrocephalus
Spinal dysraphism
UCC
Pristina
1. Introduction
The word derives from the Greek word hydrocephalus: Hydros-water cephalus-head-which means water head. Manifestation of hydrocephalus means intracranial space increased through which cerebrospinal fluid circulates. By all means spinal dysraphism, spinal defects caused due to lack of closure of the arc posterior spinal elements respectively, laminate and process Spinoza spine. Disorders occurs during early fetal development being manifested with varieties of spinal defects. The incidence of occurrence of spinal dysraphism in the U.S. ranges 2/1 000 and in Japan it behaves pathology 0.2/1 000 showing fewer. But in Kosovo this pathology 5-7 per thousand in 1 000 brought the newborn with spinal dysraphism. Based on the statistics of“WHO” show that all general congenital anomalies recorded during the birth, informed about 12.8 per thousand, it shows that the CNS congenital malformations occur in or around 20.4 per thousand in 1 000 to 2.6 children born babies with these abnormalities.
Hydrocephalus classification: Based on the life period of the event can be: hydrocephalus born, hydrocephalus gained. On the basis of anatomic aspects, physiological, and pathophysilogy distinguish this classification: anatomical: a) internal hydrocephalus b) external hydrocephalus c)combined morphological hydrocephalus: hydrocephalus partial, incomplete hydrocephalus both forms can be communicative and non-communicative hydrocephalus. Dandy classifies hydrocephalus: Form hiper-secrete hydrocephalus of obstacles in circulation, form aresoptive. In functional-based clinical criteria are divided into: active and passive hydrocephalus. Etiology factors that cause hydrocephalus are: congenital, prenatal and postnatal, subarachnoid bleeding, tumors, infections, trauma, vascular malformations. Classification of spinal dysraphism: meningocele, myelomeningocele and spina bifida occulta. Diagnosing hydrocephalus and spinal dysraphism: Diagnosing hydrocephalus and spinal dysraphism starts from intrauterine life to the observation of infants with clinical symptoms of his clinic. Diagnostic methods are: ultrasound (intrauterine), ECHO transfontanelar, X-rays of the head, the axis X-ray spinal, computerized tomography of the head and back. Magnetic resonance. FOU (fundusi the eye). Operative technique and spinal dysraphism Shanti hydrocephalus ventrikular-peritoneal-Patient’s position is horizontal instep-raiser head back in the opposite side of where to put drainage system and Shanti ventrikularatrial. Complications: Based on the time of postoperative complications, early and late, based on the type of complication,infectious, mechanical and combined based on localization: local, general and combined, based on part of system: the cranial valve, and the distal part.
Cases are handled and operated in the Neurosurgery Clinic at the Clinical Centre in Pristina in the period 2010-2012. Initially surgical treatment of spinal dysraphism subsequently intervene or monitor hydrocephalus appearance of these cases. The main aims of the paper: The cases appear in the spinal dysraphism operated by UCC, by: Year, sex, age groups and settlements; Present cases operated by the UCC spinal dysraphism under: types and localization; Division in years myelomeningocele by neurological deficit; Present cases the hydrocephalus operated and non-operated to types of spinal dysraphism; Presentation of hydrocephalus operated by acutism; appearance of complications following cases operated. Other objectives of this research are: Identification of congenital malformations during the intrauterine period, Surgery in the spinal dysraphism and hydrocephalus, neurological benefit, the ability to live independently; Forecast the possibility of reducing the birth rate with congenital malformations.
2. Materials and methods
This prospective clinical study-research includes epidemiological and congenital malformations of the spinal dysraphism and its forms are manifested by the appearance of hydrocephalus in the Neurosurgery Clinic in Pristina for the period 2010-2012. Analyzed all cases of spinal dysraphism operated in Neurosurgery Clinic in Pristina for the period 2010-2012. The results obtained are presented in tables and graphs. From statistical parameters are computed index structure, the arithmetic mean, standard deviation, and testing results is made with t-test and χ2-test. Verification testing is done on the level of confidence P<0:05 and P<0.01 respectively for the degree of error 5% or 1%.
3. Results
In the Neurosurgery Clinic at UCC since 2010-2012 were operated 55 cases of spinal dysraphism. The largest number of operations recorded in 2011 with 20 operated cases or 36.36%, while smaller in 2010 with 17 cases or 30.91% operated (Table 1 and Figure 1).

Table 1. Performance of cases of spinal dysraphism operated by the UCC, Pristina, by year, 2010-2012.
In tabular statement changes the number of patients per year. On the graph at the beginning have increased gradually over the years, which follows the rise and decline again by the end of the graph.
By sex and years, the largest number of cases of spinal dysraphism was registered in 2012 with 14 cases or 37.8%, while the small number of men in 2010 to 11 cases or 29.7%. While the female gender, the largest number of cases was recorded in 2011 with 8 cases or 44.4%, while the smallest number in 2012 with 4 cases or 22.2%.
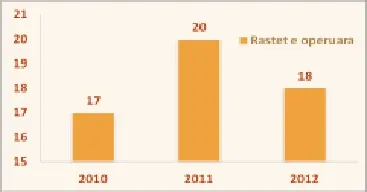
Figure 1. Graphic cases of spinal dysraphism operated by the UCC, Pristina, by year, 2010-2012.
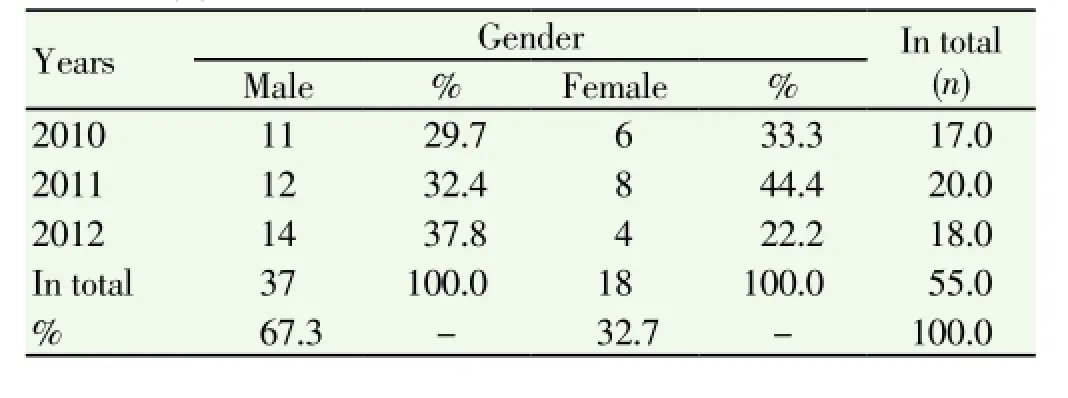
Table 2. Performance of cases of spinal dysraphism operated by the UCC, Pristina, by year and sex, 2010-2012.
Age group of patients investigated with age resulting from 0-6 months 69.1%, with 21.8% after 7-12 months of age and over 1 years to 9.1%. In graphical have 38 patients (0-6 months), 12 patients (7-12 months) and 5 patients (over 1 year). (Table 3)

Table 3. Performance of cases of spinal dysraphism operated by the UCC, Pristina, by age group, 2010-2012.
In our clinical material (Table 4) dysraphisms are investigated by localization, where the lumbo-sacral spinal axis are identified with dysraphism total 40 patients or 72.2% of cases, thorax-lumbo 12 patients or 21.8% and cervical 3 patients or 5.5%. The difference according to disease localization and by gender is high since significance P<0.001 (χ2test = 42.04).

Table 4. Performance of cases operated by the UCC dysraphism, Pristina, according to localization and sex, 2010-2012.
While the female gender were identified in a few cases, the spinal dysraphism 5 meningocele or 33.3% and 10 with spinal dysraphism myelomeningocele or 66.7% (Table 5).
While the largest number of spinal dysraphism with meningocele with lumbo-sacral localization was identified with 6 cases operated, while smaller spinal dysraphism with cervical localization meningocele with 3 cases operated (Table 6).
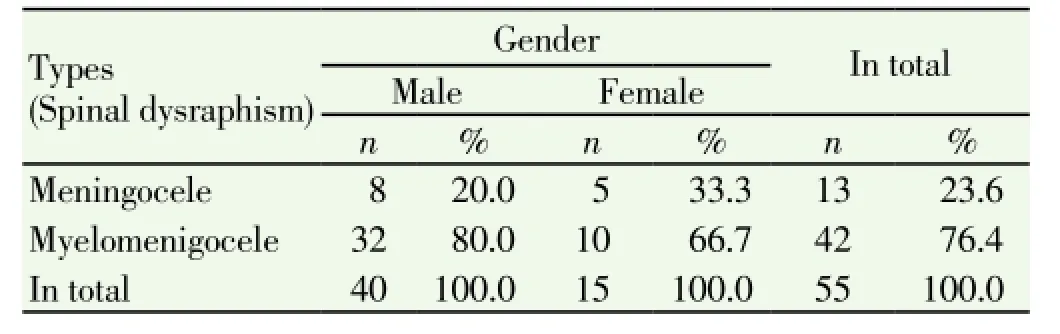
Table 5. The performance of the types of cases in spinal dysraphism operated by UCC, Pristina, by type, 2010-2012.
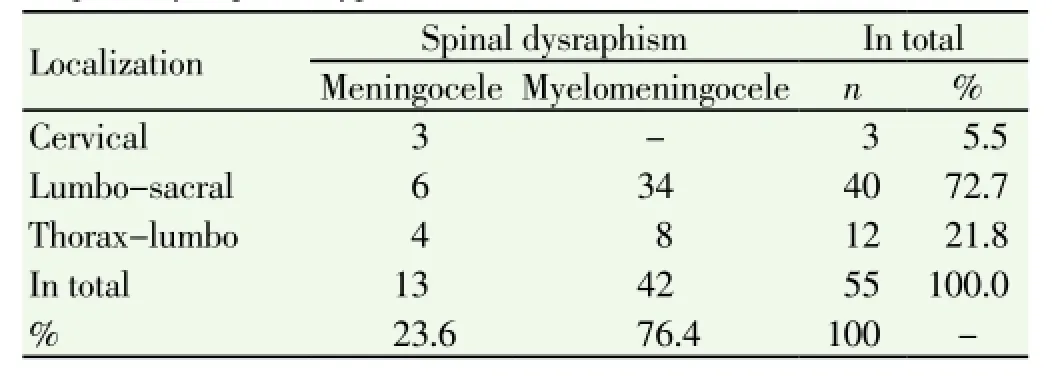
Table 6. Operating performance in UCC cases, Pristina, according localization of spinal dysraphism types , 2010-2012.
Of the total number (13 cases or 23.6%) of the spinal dysraphism meningocele, 8 cases have been identified as the hydrocephalus operated and 5 cases as hydrocephalus not operated.Whereas the total number (42 cases or 76.4%) of the spinal dysraphism myelomeningocele, 40 cases have been identified as operated hydrocephalus and two cases as non-operated hydrocephalus (Table 7).
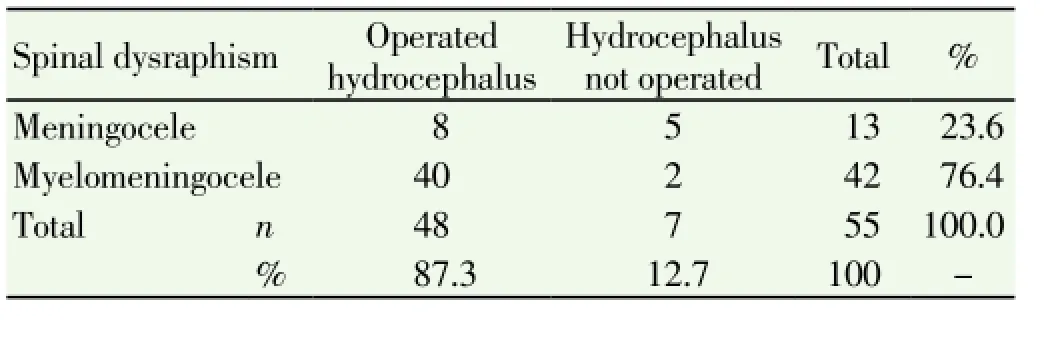
Table 7. Hydrocephalus operated and non-operated of spinal dysraphism types.
In our study six of patients had various complications. In operated patient with dysraphism respectively by myelomeningocele we had dehiscencë of the wound caused by the aggregation operators and pressure of cerebrospinal fluid.
4. Discussion
Spinal dysraphism with hydrocephalus are congenital malformations specifically stated that the percentage mentioned earlier. Based on the socio-economic circumstances of the education level of education, Kosovo, as a country (society) which remains the need to set up medical professionalism at all levels and health segments. The incidence of occurrence of spinal dysraphism in the U.S. ranges 2/1 000 and in Japan it behaves pathology 0.2/1 000showing fewer. But to us this pathology 5-7 per thousand in 1 000 brought the newborn with spinal dysraphism. Raising awareness of health requires the involvement of relevant institutions in our society in terms of awareness of the population to basic information and knowledge about health and the possibility of pregnancy in preventing transmission of the notification of these illnesses. Professionalism of staff and regional medical centers will help to reduce such occurrences. Inter professional medical cooperation enables appropriate management in terms of prevention, treatment and care for them. In the last decade in our region this malformacion increased significantly by liaising with the consequences of war from contaminating substances and the use of different drugs in pregnancy during the embryogenesis[9-11].
Brock and Sutcliffe have detected that the concentration of alpha-1-fetoprotein (AFP alpha-1-fetoprotein) in amniotic fluid substantially increases the number of children with spina bifida, anencephaly and hydrocephalus in most pregnancies. Given that the AFP crosses the placenta and can be detected in serum, serological early recovery and avoiding risk pregnancy is possible. AFP reaches maximum growth of 12 to 14 weeks of gestation, and the amniotic fluid should be examined until the 16th week[5,7,10].
Meningocele associated with a slower development of hydrocephalus where, according to our study, even after closing dysraphism, hydrocephalus can not develop. The present study strongly suggests that the growing trend of hydrocephalus may be related to prenatal diagnosis. Ultrasonography subsequent reference to these cases CAISM is due to the fact that the center is located in a referral hospital. Our study is. to close in data in Europe. Care effect when there-bag of nerves in the spine of the newborn baby, the opportunity to live it is higher if operated within the first few weeks of life. Operation enables defect covered with muscles and skin. On the other hand to children who have a majeure anomaly should be required in all systems other anomalies which may affect the treatment and the after life. To define these anomalies need wider multidisciplinary team of some profiles as pediatrician, neurologist, neurosurgeon, geneticist[1,3,7,11].
In the Neurosurgery Clinic at UCC since 2010-2012 have been operated a total of 55 cases of spinal dysraphism. The largest number of operations recorded in 2011 with 20 operated cases or 36.36%, while smaller in 2010 with 17 cases or 30.91% operated. Number of patients varies by year, with some variations of the graph, where at the beginning of the graph have increased gradually over the years, following the continuous growing and finally again with the graph cuts. By sex and years, the largest number of cases in men with spinal dysraphism was registered in 2012 with 14 cases or 37.8%, while the smallest number in 2010 with 11 cases or 29.7%. The difference according to disease localization and by gender is high since sinjifinace P<0.001 (χ2test = 42.04). In our clinical material dysraphism investigated by localization, where the lumbo-sacral to 12 patients or 21.8% and cervical to 3 patients or 5.5%. By sex and localization, with the largest number of cases in males was recorded with 26 cases with localized dysraphism lumbo-sacral or 68.4%, while the smallest number of cervical localization dysraphism with 2 cases or 5.3%. While the female gender, the largest number of cases was recorded in 14 cases with localized dysraphism lumbo-sacral or 82.4%, while the smallest number of cervical localization dysraphism with 1 case or 5.9%. The difference between myelomeningocele and meningocele according to gender, is the highest since significance P<0.001 (χ2test = 17.84). The separation of spinal dysraphism were identified by species total: 13 with spinal dysraphism meningocele or 23.6% and 42 dysraphism with spinal myelomeningocele or 76.4%, that was male dominated, in relation to female sex ratio (M:F = 40:15 occasions ).
By sex and spinal dysraphism species, the males are identified with many cases, the spinal dysraphism meningocele 8 or 20% and 32 with spinal dysraphism myelomeningocele or 80%. While the female gender were identified in a few cases, the spinal dysraphism 5 meningocele or 33.3% and 10 with spinal dysraphism myelomeningocele or 66.7%.
The largest number of cases by type of spinal dysraphism was registered to the spinal dysraphism myelomeningocele with a total of 42 cases or 76.4%, while the smallest number of spinal dysraphism with meningocele with 13 cases or 23.6%. While according to localization of these types of spinal dysraphism, the largest number of spinal dysraphism with myelomeningocele with lumbo-sacral localization was recorded with 34 cases operated, while the smallest number with spinal dysraphism myelomeningocele with thorax-lumbo with 8 cases operated. While the largest number of spinal dysraphism with meningocele with lumbo-sacral localization was identified with 6 cases operated, while smaller spinal dysraphism with cervical localization meningocele with 3 cases operated. The meningocele are registered 8 hydrocephalus (16.7%) of 13 the spinal dysraphism meningocele (23.6%). While the myelomeningocele 40 hydrocephalus (83.7%) of the 42 spinal dysraphism myelomeningocele (76.4%). Hydrocephalus difference between operated and non-operated significance is high as P<0.001 (χ2test = 50.88). Patients with hydrocephalus notice investigated by surgical treatment (hydrocephalus operated) with a total of 48 cases or 87.3% and conservative (non-operated hydrocephalus) with a totalof 7 cases or 12.7%.
Of the total number (13 cases or 23.6%) of the spinal dysraphism meningocele, 8 cases have been identified as operated hydrocephalus and 5 cases of non-operated hydrocephalus. While the total number (42 cases or 76.4%) of the spinal dysraphism myelomeningocele, 40 cases have been identified as hydrocephalus the two cases operated and non-operated as hidrocephalus. The difference between hydrocephalus operated by the myelomeningocele acutism significance is very high as P<0.001 (χ2test = 51.14). Hydrocepahlus surgical treatment has its acutism course, which is presented in the form hiper-acute in 9 patients or 16.4% initially operated by hydrocepahlus before closing spinal dysraphism. Hydrocephalus acute form to have one month to 29 patients or 52.7%, while the hydrocephalus subacute form of operating from 6-12 months to 17 patients have or 30.9%.
In our study of six patients had various complications. In a operated patient with dysraphism respectively by myelomeningocele we had dehiscence of the wound caused by the aggregation operators and cerebrospinal pressure fluid Disfunction of Shanti ventrikulo - the first peritoneal patients manifested both in the cranial with cranial closure valve and ventricular catheter and in the distal portion of the catheter peritoneal closure. Shanti Eksterioizm where the body rejects foreign body system as we had the first patients. Shanti meningitis due to infection or eventual reduction in immune intervention, was warned to 5 patients. Bilateral subdural hematoma due to excessive absorption of the system is evidenced in 1 patient.
Recommendations
Of all pregnant women are required to be under control of the gynecologist in the first quarter and the second half of pregnancy. In case of doubt it amniocenteza for detection of alpha-1 fetoprotein. All pregnant women to control the amount of serum folic acid. Women in the age of deferred were planning pregnancy should consume 0.4 mg of folic acid every day. To children who have a majeure anomalie should be required on all systems other anomalies, and for defining these anomalies need wider multidisciplinary team of some profiles as pediatrician, neurologist, neurosurgeon, geneticist. Cytogenicity be tested specifically to women recessive genetic predisposition gene in the X chromosome Sy Bickerc rds-Adams-Edwards.
Conflict of interest statement
We declare that we have no conflict of interest
[1] Treanor Brian. Aspects of alterity: Levinas, marcel, and the contemporary debate. Fordham: Fordham University Press; 2006, p. 41.
[2] Engle Eric. Lex Naturalis, Ius Naturalis. Law as positive reasoning & natural rationality. Melbourne: The Rlias Clark Group; 2010, p. 75.
[3] Miller N, Lacroix EM, Backus J. MEDLINE plus: building and maintaining the National Library of Medicine’s consumer health web service. Bull Med Libr Assoc 2000; 88(1): 11-17.
[4] Marill JL, Miller N, Kitendaugh P. The MedlinePlus public user interface: studies of design challenges and opportunities. J Med Libr Assoc 2006; 94(1): 30-40.
[5] T. Kohl, A. Kawecki, J. Degenhardt, R. Axt-Fliedner, B. Neubauer. Early neurological findings in 20 infants after minimally-invasive fetoscopic surgery for spina bifida at the University of Giessen 2010-2011. Ultrasound Obstet Gynecol 2012; 40: 9.
[6] Degenhardt J, Schürg R, Kawecki A, Pawlik M, Enzensberger C, Stressig R, et al. Mütterliches Outcome nach minimal-invasivem verschluss einer spina bifida. Ultraschall Med 2012; 33: S96.
[7] Degenhardt J, Schürg R, Kawecki A, Pawlik M, Enzensberger C, Stressig R, et al. Maternal outcome after minimally-invasive fetoscopic surgery for spina bifida. The Giessen experience 2010-2012. Ultrasound Obstet Gynecol 2012; 40(Suppl 1): 9.
[8] Neubauer B, Degenhardt J, Axt-Fliedner R, Kohl T. Frühe neurologische Befunde von Säuglingen nach minimal-invasivem fetoskopischen verschluss ihrer spina bifida aperta. Z Geburtsh Neonat 2012; 216: 87.
[9] Kohl T, Kawecki A, Degenhardt J, Axt-Fliedner R, Neubauer B. Early neurological findings in 20 infants after minimally-invasive fetoscopic surgery for spina bifida at the University of Giessen 2010 - 2011. Ultrasound Obstet Gynecol 2012; 40(Suppl. 1): 9
[10] Kohl T, Schürg R, Maxeiner H, Tchatcheva K, Degenhardt J, Stressig R, et al. Partial carbon dioxide insufflation (PACI) during fetoscopic surgery on 60 fetuses with spina bifida. Ultrasound Obstet Gynecol 2012; 40(Suppl. 1): 73-74
[11] Kohl T, Kawecki A, Degenhardt J, Axt-Fliedner R. Preoperative sonoanatomic examination of fetal spina bifida permits prediction of surgical complexity during subsequent minimally-invasive fetoscopic closure. Ultrasound Obstet Gynecol 2012; 40(Suppl. 1): 8.
[12] R.J. Verbeek, A. Heep. Fetal endoscopic myelomeningocele closure preserves segmental neurological function. Develop Med Child Neurol 2012; 54(1): 15-22.
[13] Kohl T, Gembruch U. Current status and prospects of fetoscopic surgery for spina bifida in human fetuses. Fetal Diagn Ther 2008; 24(3): 318-320.
[14] Holmbeck GN, DeLucia C, Essner B, Kelly L, Zebracki K, Friedman D, et al. Trajectories of psychosocial adjustment in adolescents with spina bifida: A 6-year, four-wave longitudinal follow-up. J Consult Clin Psychol 2010; 78(4): 511-525.
ment heading
10.1016/S2221-6189(14)60009-3
*Corresponding author: Mr.Sc. Dr. Besnik Elshani, Str. Ulpiana A1 / 4, 10000 Pristina, The Republic of Kosovo.
E-mail: besniku71@yahoo.com
杂志排行
Journal of Acute Disease的其它文章
- Acute reaction to erroneous injection of adrenaline to the patients with hyperthyroidism
- Acute hepatitis with observed increased blood phenytoin level: a case study
- The value of C-reactive protein in emergency medicine
- Attitude and perception of junior resident doctors’ regarding antibiotic resistance - A pilot study
- MRSA toxic shock syndrome associated with surgery for left leg fracture and co-morbid compartment syndrome
- Stromal opacity secondary to preservative in dilating drops - A case report and review of literature
