Acute temporal lobe infarction in a young patient associated with marijuana abuse: An unusual cause of stroke
2014-03-17TaylanInalAtamansezlemksalErolArmaganSuleAydFatmaOzdemir
Taylan Inal, Ataman Köse, Özlem Köksal, Erol Armagan, Sule A. Aydın, Fatma Ozdemir
1Department of Emergency Medicine, Sevket Yılmaz Education and Research Hospital, Bursa, Turkey
2Department of Emergency Medicine, Faculty of Medicine, Uludag University, Bursa, Turkey
Corresponding Author:Ataman Köse, Email: ataberk76@yahoo.com.tr
Acute temporal lobe infarction in a young patient associated with marijuana abuse: An unusual cause of stroke
Taylan Inal1, Ataman Köse1, Özlem Köksal2, Erol Armagan2, Sule A. Aydın2, Fatma Ozdemir1
1Department of Emergency Medicine, Sevket Yılmaz Education and Research Hospital, Bursa, Turkey
2Department of Emergency Medicine, Faculty of Medicine, Uludag University, Bursa, Turkey
Corresponding Author:Ataman Köse, Email: ataberk76@yahoo.com.tr
BACKGROUND:Cardiovascular or cerebrovascular events associated with drug abuse have been frequently reported, particularly in young patients. The drugs include generally cocaine, heroin, and amphetamines. Although marijuana is among the widely used narcotics in the world, stroke associated with the marijuana use is infrequently reported.
METHODS:Stroke caused by the use of marijuana was investigated in a 23-year-old man and the importance of inquiry of drug abuse in case of stroke was emphasized.
RESULTS:The patient was treated for 7 days in a follow-up, but he was not recovered. The patient was discharged in his existing condition and was directed for physiotherapy and rehabilitation.
CONCLUSION:Ischemic stroke is associated with drug abuse and/or substance use, mainly cannabinoids and amphetamines, particularly in young patients.
Marijuana abuse; Stroke; Emergency medicine
INTRODUCTION
Obtained from Cannabis sativa containing delta-9-tetrahydrocannibol (THC), marijuana is one of the most commonly abused substances in the world, with increased use among young people. This plant produces psychoactive chemicals known as "cannabinoids" and more than 60 kinds of them are known. The most wellknown substance is 8–9-THC.[1–3]Cannabinoids may exert their effects on the brain of humans.[4]
The desired effects of cannabis are euphoria, self-confidence, relaxation, and goodness. Their psychological effects start in minutes and last for 2–3 hours.[5]They may cause distraction including shortterm memory loss. The effects on the respiratory system, central nervous system, and psychology are usually non-permanent.[2,6]Stroke associated with drug abuse has been reported in some cases,[7,8]with an incidence of 2%–39% in young patients.[9]Marijuana is the most widely abused drug, but only few reports are available on stroke associated with it. This report aims to present a case of stroke in a young man because of the use of marijuana.
CASE REPORT
A 23-year-old man was admitted to the emergency department (ED) because of somnolence and weakness in the right side of the body. Except for smoking cigarette, classical risk factors for stroke/embolism were absent. He did not receive any regular medication for known systemic disease and he had no family history of cerebro-vascular diseases. His initial vital signs were: arterial blood pressure 130/80 mmHg, pulsation 90/min, temperature 36.8oC, and oxygen saturation in room air 98. ECG showed normal sinusrhythm of 80 per minute. On neurological examination, he was non-cooperative, disoriented, and aphasic. There existed hemiparesis (1/5 motor power) in his right upper extremity and (2/5 motor power) in the lower extremities. Right nasolabial sulcus was lost and Babinski test was positive on the right side. No feature was observed on other examinations. No abnormality was detected by laboratory examinations in the ED (tests for blood count, coagulation times, electrolytes, glucose, ammonia level, liver and renal function, arterial blood gas, and carboxyhemoglobin level). Alcohol intoxication was excluded for a normal blood alcohol level. In a screening test (competitive fluorescence immunoassay; The Triage[R]TOX Drug Screen) urine samples were negative for benzodiazepines, barbiturates, methamphetamine, cocaine, opioids, phencyclidine, and tricyclic antidepressants. However, THC metabolites were detected as positive in the same toxicological screening. Cranial tomography (CT) scan was normal on admission, but a diffusion-weighted magnetic resonance imaging (DWMRI) detected an acute infarct sized 4 cm×5 cm in the temporal lobe on the left side (Figures 1, 2).
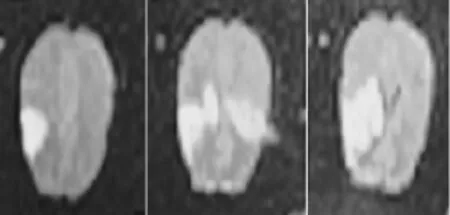
Figure 1. Diffusion-weighted cranial magnetic resonance imaging of the patient.

Figure 2. Cranial magnetic resonance imaging of the patient.
With a diagnosis of occlusive type cerebrovascular disease, the patient was given heparin and 300 mg of acetylsalicylic acid in addition to anti-edema treatment and a neurological consultation. The patient was examined by neurologists in the ED and admitted to the neurology ward. After anti-edema treatment for 7 days, he was not recovered clinically. He was discharged home in his existing condition and received physiotherapy and rehabilitation treatment.
DISCUSSION
Cerebrovascular ischemia and infarction might be related to the use of marijuana, but its mechanism is not clear. Probably, vasospasm caused by vasoconstrictive effect of THC is responsible for this mechanism. Others might be systemic hypotension, instable cerebral autoregulation, instable cerebral blood flow, vacuities, cerebral vasoconstriction syndrome, and cardiac embolism with atrial fibrillation.[2,3,7,8,10]Although a few of these mechanisms may coexist, evidence explaining the causes of stroke needs to be found.
It was reported that THC might contribute to recurrent stroke because of its vasoconstrictive effects and resultant instable cerebral blood flow.[6,11,12]Long-term use of marijuana in young people may cause serious damage to the cerebrovascular system, and toxicological screening should be done if necessary. Moreover, marijuana abuse causes systemic hypertension and damage of vasomotor reflexes and the central nervous system.[10,13]
Geller et al[3]reported three cases of cerebellar infarction caused by marijuana abuse. Cerebellar infarction was found by biopsy or necropsy and infiltration of inflammatory cells was detected in the cases. Cerebellar and brainstem stroke occurred because of cerebral edema in two cases, who died eventually. Obviously, marijuana abuse causes hypotension, deteriorates vasomotor reflexes, and reduces cerebral blood flow. Thus the low collateral blood flow affects the cerebellum and causes cerebellar ischemia.[3]Singh et al[8]found cerebral infarction in 17 cases of focal neurological deficit after the use of cannabis. Another study reported a 35-year-old man with unconsciousness, agitation and acute right hemiplegia after the use of cannabis, and MRI and MR angiography demonstrated an acute infarction of the middle cerebral artery.[6]Trojak et al[13]reported a 24-year-old Caucasian man in a deeply comatose nonreactive state after cannabis use. A MRI scan of his brain showed bilateral multiple ischemic infarcts. Mateo et al[7]also reported a patient who suffered three ischemic strokes immediately after cannabis consumption. Cranial MRI revealed two acute ischemic infarcts (in the left temporal lobe and the right parietal lobe). In our case, the patient was unconscious and had right hemiplegia after cannabisuse. Cranial MRI showed acute ischemic infarcts over the left temporal lobe, consistent with his neurological deficit.
In conclusion, ischemic stroke is associated with drug abuse and/or substance use (mainly cannabinoids and alcohol), particularly in young adult patients. Hence, toxicological screening is necessary for patients with unconsciousness and neurological deficit who presented to the ED.
Funding:None.
Ethical approval:Not needed.
Conflicts of interest:The authors declare that there is no conflict of interest.
Contributors:Inal T and Kose A contributed to the study design, drafting of the manuscript, wrote the manuscript and organized the research. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
1 Klein TW, Newton C, Larsen K, Lu L, Perkins I, Nong L, et al. The cannabinoid system and immune modulation. J Leukoc Biol 2003; 74: 486–496.
2 Thanvi BR, Treadwell SD. Cannabis and stroke: is there a link? Postgrad Med J 2009; 85: 80–83.
3 Geller T, Loftis L, Brink DS. Cerebellar infarction in adolescent males associated with acute marijuana use. Pediatrics 2004; 113: e365–70.
4 Barinaga M. Neurobiology. How cannabinoids work in the brain. Science 2001; 291: 2530–2531.
5 Ashton CH. Adverse effects of cannabis and cannabinoids. Br J Anaesth 1999; 83: 637–649.
6 Singh NN, Pan Y, Muengtaweeponsa S, Geller TJ, Cruz-Flores S. Cannabis-related stroke: case series and review of literature. J Stroke Cerebrovasc Dis 2012; 21: 555–560.
7 Mateo I, Pinedo A, Gomez-Beldarrain M, Basterretxea JM, Garcia-Monco JC. Recurrent stroke associated with cannabis use. J Neurol Neurosurg Psychiatry 2005; 76: 435–437.
8 Singh NN, Pan Y, Muengtaweeponsa S, Geller TJ, Cruz-Flores S. Cannabis-related stroke: case series and review of literature. J Stroke Cerebrovasc Dis 2012; 21: 555–560.
9 Sloan MA, Kittner SJ, Rigamonti D, Price TR. Occurrence of stroke associated with use/abuse of drugs. Neurology 1991; 4: 1358–1364.
10 Renard D, Taieb G, Gras-Combe G, Labauge P. Cannabisrelated myocardial infarction and cardioembolic stroke. J Stroke Cerebrovasc Dis 2012; 21: 82–83.
11 Iversen L. Cannabis and the brain. Brain 2003; 126: 1252–1270.
12 Finsterer J, Christian P, Wolfgang K. Occipital stroke shortly after cannabis consumption. Clin Neurol Neurosurg 2004; 106: 305–308.
13 Trojak B, Leclerq S, Meille V, Khoumri C, Chauvet-Gelinier JC, Giroud M, et al. Stroke with neuropsychiatric sequelae after cannabis use in a man: a case report. J Med Case Rep 2011; 30: 264.
Received March 19, 2013
Accepted after revision July 28, 2013
World J Emerg Med 2014;5(1):72–74
10.5847/ wjem.j.issn.1920–8642.2014.01.013
杂志排行
World journal of emergency medicine的其它文章
- Wilderness medicine
- Lean techniques for the improvement of patients'flow in emergency department
- The knowledge level offinal year undergraduate health science students and medical interns about cardiopulmonary resuscitation at a university teaching hospital of Northwest Ethiopia
- Strategic planning and designing of a hospital disaster manual in a tertiary care, teaching, research and referral institute in India
- Effects of early rehabilitation therapy on patients with mechanical ventilation
- Bispectral index in predicting the prognosis of patients with coma in intensive care unit
