Significance of blood pressure variability in patients with sepsis
2014-03-17
Department of Emergency Medicine, Tianjin Medical University General Hospital, Tianjin 300052, China
Corresponding Author:Nishant Raj Pandey, Email: nishantrpandey@gmail.com
Significance of blood pressure variability in patients with sepsis
Nishant Raj Pandey, Yu-yao Bian, Song-tao Shou
Department of Emergency Medicine, Tianjin Medical University General Hospital, Tianjin 300052, China
Corresponding Author:Nishant Raj Pandey, Email: nishantrpandey@gmail.com
BACKGROUND:This study was undertaken to observe the characteristics of blood pressure variability (BPV) and sepsis and to investigate changes in blood pressure and its value on the severity of illness in patients with sepsis.
METHODS:Blood parameters, APACHE II score, and 24-hour ambulatory BP were analyzed in 89 patients with sepsis.
RESULTS:In patients with APACHE II score>19, the values of systolic blood pressure (SBPV), diasystolic blood pressure (DBPV), non-dipper percentage, cortisol (COR), lactate (LAC), platelet count (PLT) and glucose (GLU) were significantly higher than in those with APACHE II score ≤19 (P<0.05 ), whereas the values of procalcitonin (PCT), white blood cell (WBC), creatinine (Cr), PaO2, C-reactive protein (CRP), adrenocorticotropic hormone (ACTH) and tumor necrosis factor α (TNF-α) were not statistically significant (P>0.05). Correlation analysis showed that APACHE II scores correlated significantly with SBPV and DBPV (P<0.01, r=0.732 and P<0.01, r=0.762). SBPV and DBPV were correlated with COR (P=0.018 and r=0.318; P=0.008 and r=0.353 respectively). However, SBPV and DBPV were not correlated with TNF-α, IL-10, and PCT (P>0.05). Logistic regression analysis of SBPV, DBPV, APACHE II score, and LAC was used to predict prognosis in terms of survival and non-survival rates. Receiver operating characteristics curve (ROC) showed that DBPV was a better predictor of survival rate with an AUC value of 0.890. However, AUC of SBPV, APACHE II score, and LAC was 0.746, 0.831 and 0.915, respectively.
CONCLUSIONS:The values of SBPV, DBPV and non-dipper percentage are higher in patients with sepsis. DBPV and SBPV can be used to predict the survival rate of patients with sepsis.
Sepsis; Systolic blood pressure variability; Diastolic blood pressure variability; APACHE II score; Inflammatory factor
INTRODUCTION
Blood pressure (BP) is the pressure exerted by circulating blood upon the walls of blood vessels. The BP values are the end product of both intrinsic (cardiovascular, renal, endocrinal system) and extrinsic factors. Due to these complex mechanisms, BP undergoes continuous changes over a period of time. With the invention of automatic noninvasive ambulatory BP monitoring (ABPM) devices, sensing blood pressure variability (BPV), a significant marker of this complex mechanism, has been easy. These variables can be recorded in a specific interval, measuring both endogenous and exogenous variability, over a period varying from few hours to several weeks. These ABPM recorded variabilities are of much significance in determining various risk facts as compared with BP obtained by doctors or nurses in both outpatient department and inpatient department.[1]These variables can be recorded in a specific interval, measuring both endogenous and exogenous variabilities, over a period varying from fewhours to several weeks. Cross-sectional studies have reported that 24-hour BPV is associated with target-organ damage, independent of mean BP.[2–5]
Sepsis may cause numerous endocrinological alterations that may play a significant role in prognosis of the disease.[6–9]One of the responses is the activation of hypothalamopituitary-adrenal axis, which increases the cortisol (COR) production. However, this enhanced plasma cortisol level is insufficient to control the inflammatory response. We have realized that there is a significant relationship between body's response to sepsis, body's metabolism, and the immune and neroendocrine systems. In conclusion, there is evidence that central nervous system (CNS) controls body's response to inflammation. One of the best 'physiomarkers' that can be studied through analysis of blood pressure is the blood pressure variability (BPV), that is the variability of both systolic blood pressure (SBPV) and diasystolic blood pressure (DBPV).
In this study, we observed the characteristics of BPV and sepsis and investigated changes in blood pressure and the severity of illness in patients with sepsis.
METHODS
This study included patients over 18 years old admitted to the Emergency Intensive Care Unit diagnosed with sepsis as defined by the American College of Chest Physicians and the Society of Critical Care Medicine Conference Consensus Committee.[10]Exclusion criteria included corticosteroid use in the past three months or its requirement as part of the treatment at admission, administration of etomidate, end-stage cancer, AIDS, chronic renal failure requiring hemodialysis support, cirrhosis (Child–Pugh class C), pregnancy, stage II hypertension or limited life care support. We also excluded patients with septic shock, refractory septic shock and multiple organ dysfunction syndromes as defined by the American College of Chest Physicians and the Society of Critical Care Medicine Conference Consensus Committee.[10]The Department of Emergency Medicine Review Board of Tianjin Medical University General Hospital approved the study protocol and informed consents were obtained from patients. The patients did not have blood drawn exclusively for study purposes. Blood samples were taken from the patients according to the protocol approved by the ethics committee of the hospital.
Between November 2011 and April 2012, 89 patients (46 males, 43 females) who had been diagnosed with sepsis were included in this study. On their admission to the ED, the following variables were recorded: 1) general characteristics including age, sex and diagnosis; 2) physiological parameters including temperature, heart rate, respiratory rate; 3) prognosis evaluated by the 28-day mortality rate; 4) APACHE II score calculated within 24 hours; 5) blood parameters including complete blood count, liver function test, kidney function test, serum procalcitonin level, electrolytes, blood gas analysis, C-reactive protein (CRP) serum level, erythrocyte sedimentation rate (ESR) serum level, plasma cortisol level, adrenocorticotropic hormone (ACTH) serum level were drawn and analyzed at the laboratory of Tianjin Medical University General Hospital.
All the patients underwent 24-hour ABPM within 48 hours after admission using a non-invasive monitor (MOBIL-O-GRAPH, IEM, Germany). The BP cuff was fitted to the participant's nondominant arm with cuff size determined by upper arm circumference. BP measurements were obtained at 30-minute intervals during the day (6:00 am–10:00 pm) and 60-minute intervals at night (10:00 pm–6:00 am). Participants were instructed not to exercise prior to or during the 24-hour BP monitoring period and to pause momentarily and maintain their body position during each BP measurement. Only recordings of good technical quality (>80% of valid BP measurements) were included infinal analyses. BP variability was calculated as the standard deviation of mean systolic, diastolic, mean BP, and pulse pressure. Mean systolic and diastolic BP was calculated as an overall 24-hour average for each patient.
The acute physiology and chronic health evaluation (APACHE) II score is a well-known disease severity index for hospitalized adults, which is related to the prediction of mortality.[11,12]After the patient was admitted, APACHE II score was calculated within 24 hours. According to the score, the patients were divided into two groups, namely APACHE II score>19 and APACHE score ≤19.[13]
Data were analyzed using SPSS version 11.0. Categorical variables were described in terms of frequencies and percentages. The distribution of all variables was examined using the Shapiro-Wilk test of normality. The normally distributed measurements were expressed by mean±SD, the non-normally distributed data were expressed in terms of median and interquartile range. The normally distributed measurements were compared using independent samples t test for two groups and ANOVA for three groups. However, nonparametric tests were performed for the non-normallydistributed results. Spearman's rank-order correlation coefficient was used to examine the strength of relationships between the results. Logistic regression analysis was performed to analyze the risk factors affecting the higher APACHE II score. Receiver operating characteristic curve and calculation of the area under the curve analysis were used to determine the prognosis of patients. A value of P<0.05 was considered statistically significant.
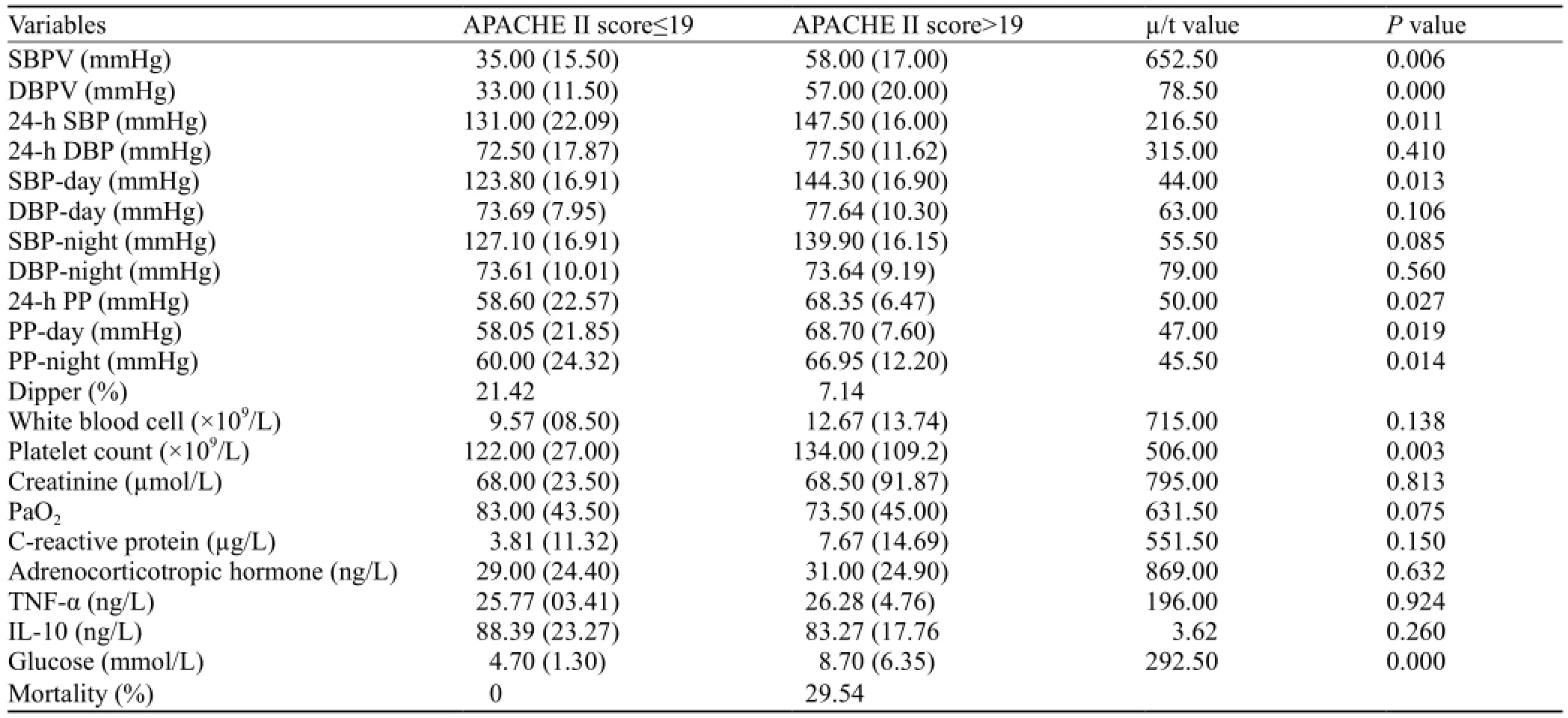
Table 1. Comparison of the APACHE II score≤19 group and APACHE II score>19 group (median: interquartile range; mean: standard deviation)
RESULTS
Baseline patient characteristics
In the 89 patients with a mean age of 67.8±18.3 years (range, 18 to 93 years), 46 males and 43 females, the predominant causes of sepsis were pneumonia (49), urinary tract infection (11), pleuritis (6), intestinal infection (4), cholecystitis (4), central nervous system infection (2), soft tissue infection (5), and other infection (8).
Assessment of ABPM
Data obtained from each ABPM were adequate for interpretation. The number of successful reading for both systolic blood pressure and diastolic blood pressure was 54 (60.7%). The overall medium value of SBP and DBP was 145.25 mmHg and 77.50 mmHg respectively. The maximum and minimum values of SBP were 177 mmHg and 86 mmHg, whereas those of DBP were 111 mmHg and 65 mmHg. The skewness value of SBP was –0.687 and that of DBP was 0.876. The Kurtosis values of SBP and DBP were 0.848 and 0.796, respectively.
Comparisons between the APACHE ll score>19 group and APACHE ll score ≤19 group
Data obtained from each blood report were adequate for interpretation (Table 1).
Correlation analysis of severity of the disease in sepsis patients and BPV
Spearman's rank-order correlation coefficientanalysis showed that APACHE II scores correlated significantly with SBPV and DBPV (Table 2).
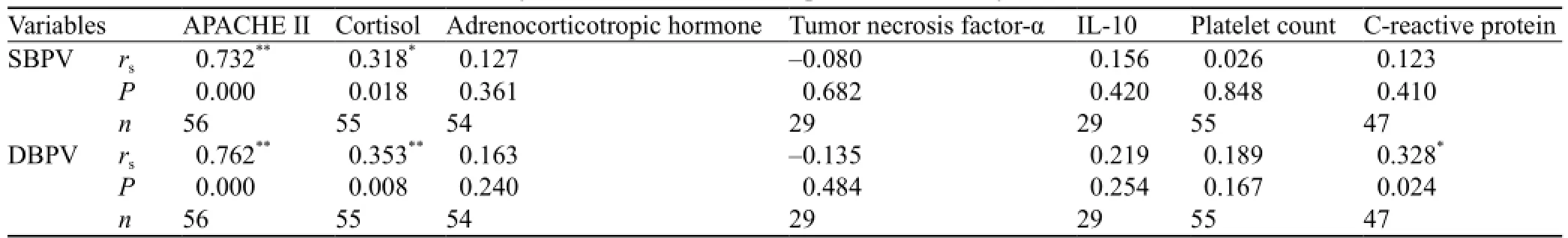
Table 2. Correlation of APACHE II score with systolic and diastolic blood pressure variability and various biomarkers
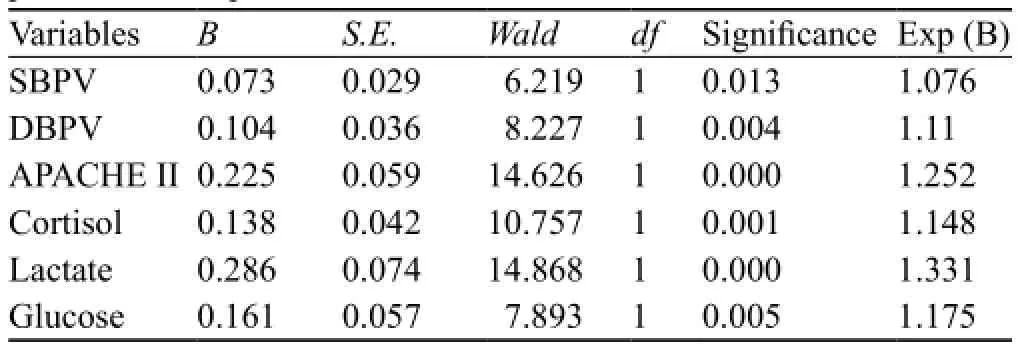
Table 3. Logistic regression analysis of factors affecting prognosis in patients with sepsis
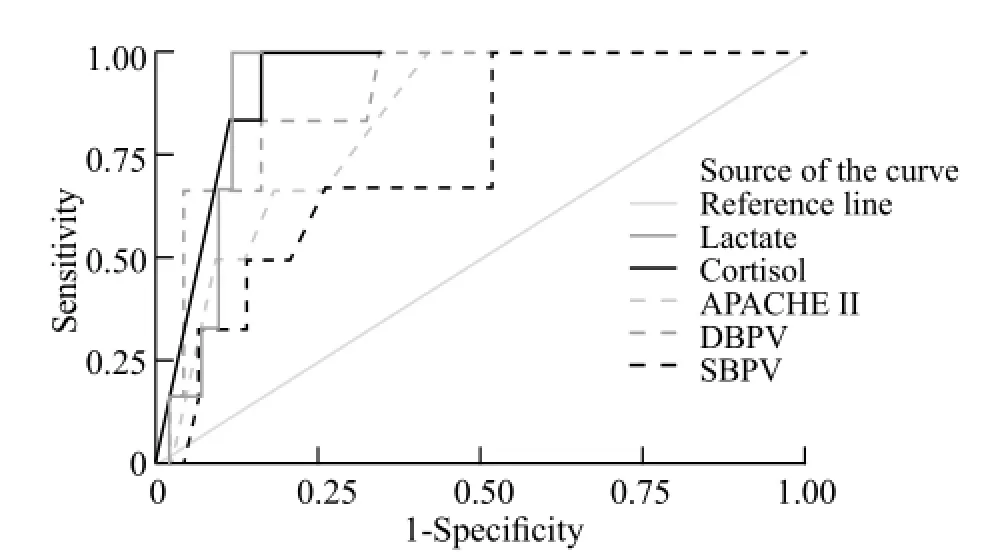
Figure 1. Receiver operating characteristic curve analyses of SBPV, DBPV, APACHE II, cortisol and lactate.
Logistic regression analyses of factors affecting prognosis in sepsis
We used binary logistic regression to evaluate possible associations between BPV and prognosis. All variables were separately analyzed (Table 3).
Receiver operator curve analysis of factors affecting prognosis in patients with sepsis
We compared SBPV, DBPV, APACHE II, lactate (LAC ) and COR to predict prognosis of patients who were alive and deaths by using receiver operating characteristics (Figure 1).
DISCUSSION
Although hypertension has been recognized as the predictor of target-organ damage, the role of BPV in the diagnosis and prognosis of sepsis is a new concept. The 24-hour BPV, which is the value of both external stimulation and cardiovascular control, can provide evidence of cardiovascular complication and possible end-organ damage.[14]Measurement of BP values varies significantly because of various factors including technical skills and accuracy of equipments also in addition to subjective factors such as stress and anxiety. However, the significance of BPV has been studied only in the hypertensive patients,[15]the general population[16]not in those with sepsis. The influence of BPV and its relationship with the severity of sepsis is still not clear. To our knowledge, this is the first study to observe the characteristics of BPV and sepsis and to investigate changes in BP and its value on the severity of illness in patients with sepsis.
Several pathophysiological mechanisms of BPV are thought to be of clinical significance. But the exact mechanisms have not been elucidated clearly. The best elucidation should be the influence of the neuroendocrine-sympatatic nervous system on sepsis. The relationship between the neuroendocrine and immune systems is well known, it has been proved that these systems use similar ligands and receptors to establish an intra- and inter-network of communication. Therefore, the communication between these systems is essential to a good health.[17]
Patients with sepsis have excessive and systemic inflammation characterized by high levels of C-reactive protein, cytokine interleukin and pro-calcitonin.[18]The xcessive inflammation in sepsis is harmful to the host. It is known that increased concentrations of tumor necrosis factor[19]and cytokine can predict the mortality of patients with sepsis.[20]It is uncertain whether inflammation in sepsis patients is the main cause of death. Despite inflammation, patients with sepsis have suppression signs of the adaptive immune response. It is known that patients with sepsis are unable to clear their original infection and are highly susceptible to secondary infection.[21]These observations have led to a new theory that patients with sepsis have increased inflammation but with time there is a decrease in the immunosuppressive state.[22]Therefore, we conclude that the neuroendrocine and immune systems play a vital role in the prognosis of patients with sepsis.
Some hormonal and neuro-peptide mediators contribute to the link between the endocrine, central nervous and immune systems through specific axes of interactions like hypothalamic-pituitary-adrenal (HPA) axis, hypothalamic–pituitary–gonadal (HPG) axis, hypothalamic-pituitary-thyroid (HPT) axis and human growth hormone (HGH) axis. Autonomic nervous system (ANS) also intercommunicates with the lymphoid system by releasing norepinephrine and acetylcholine from the sympathetic and parasympathetic nerves. Thus, the networks for multidirectional intercommunications exist in the human body allowing the transmissions of signalsbetween these systems during sepsis.
The nerves of sympathetic nervous system (SNS) have been shown to innervate lymphoid organs by which the CNS can influence the immune system during the process of sepsis. During the process, SNS is stimulated and the neurotransmitter and norepinephrine are released into the lymphoid microenvironment. The autonomic nervous system and its sympathetic arm play important roles in the regulation of blood pressure.[23,24]Their role in the short-term regulation of blood pressure, especially in responses to transient changes in arterial pressure is well known.[25]
In our study comparing two groups of APACHE II scores, the severity index and the values of SBPV, DBPV, COR, LAC, latelet count (PLT) and glucose (GLU) were statistically significant. Further analysis revealed that in the APACHE II score >19 group, the values of SBPV and DBPV were significantly higher than those in another group. We also noticed that other biomarkers like COR had higher values in the APACHE II score >19 group. This finding indicates that when the severity of disease increases in sepsis patients, the values of both SBPV and DBPV are increased. Moreover, the mortality rate was significantly higher (29.54% vs. 0%) in the APACHE II score >19 group than in the APACHE II score <19 group. Non Dipper percentages (92.86%) were high in the APACHE II score >19 group which had a higher mortality rate (29.54%) than the APACHE II score ≤19 group (non dippers: mortality; 78.58%:0%). Since the dipper status varies, it is difficult to detect its relationship with mortality by a single recording.
Spearman's rank-order correlation coefficient analysis showed that the two groups of APACHE II score were positively correlated with SBPV and DBPV. This indicated that when APACHE II score increased, blood pressure varied in our patients. Increased scores may also indicate increased inflammation of patients; therefore we conclude that inflammation during sepsis should have played a vital role in the regulation of BP. Interestingly, receiver operating characteristic curve also illustrated that DBPV was a good predictor of survival rate as compared to SBPV and APACHE II score. Further analysis showed that AUC value for SBPV was 0.746, DBPV was 0.890, and APACHE II score was 0.831. APACHE II score as an index for disease severity for hospitalized adults was related to the mortality of critically ill patients.[13]We conclude that DBPV and SBPV are good indexes of disease severity for hospitalized critically ill patients.
Limitations exist in our study. The study lacked the design of a control group because of the following reasons. The sample size of this study was small. This study was conducted to create a homogenous group to ensure lack of confounding variables. The measure of BP variability was complicated and further studies on ambulatory beat-to-beat measures of BP and inflammation in sepsis are needed. Moreover, this study could not detect the longitudinal effects of infection on sepsis and BPV. Finally, inadequate 24-hour ABPM was used in a few patients.
Funding:None.
Ethical approval:The Department of Emergency Medicine Review Board of Tianjin Medical University General Hospital approved the study protocol.
Conflicts of interest:The authors declare that there is no conflict of interest.
Contributors:Pandey NR proposed the study, analyzed the data and wrote thefirst draft. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
1 O'Brien E. Ambulatory blood pressure measurement: a trove of hidden gems? Hypertension 2006; 48: 364–365.
2 Mancia G, Parati G, Hennig M, Flatau B, Omboni S, Glavina F, et al. Relation between blood pressure variability and carotid artery damage in hypertension: baseline data from the European Lacidipine Study on Atherosclerosis (ELSA). J Hypertens 2001; 19: 1981–1989.
3 Li WY, Wang XH, Lu LC, Li H. Discrepancy of blood pressure between the brachial artery and radial artery. World J Emerg Med 2013; 4: 294–297.
4 Parati G, Pomidossi G, Albini F, Malaspina D, Mancia G. Relationship of 24-hour blood pressure mean and variability to severity of target-organ damage in hypertension. J Hypertens 1987; 5: 93–98.
5 Tatasciore A, Renda G, Zimarino M, Soccio M, Bilo G, Parati G, et al. Awake systolic blood pressure variability correlates with target-organ damage in hypertensive subjects. Hypertension 2007; 50: 325–332. Epub 2007 Jun 11.
6 Annane D, Sébille V, Charpentier C, Bollaert PE, François B, Korach JM, et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA 2002; 288: 862–871.
7 Ren HS, Gao SX, Wang CT, Chu YF, Jiang JJ, Zhang JC, et al. Effects of high-volume hemofiltration on alveolararterial oxygen exchange in patients with refractory septic shock. World J Emerg Med 2011; 2: 127–131.
8 Cooper MS, Stewart PM. Corticosteroid insufficiency in acutely ill patients. N Engl J Med 2003; 348: 727–734.
9 Briegel J. Hydrocortisone and the reduction of vasopressors in septic shock: therapy or only chart cosmetics? Intensive Care Med 2000; 26: 1723–1726.
10 No authors listed. American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 1992; 20: 864–874.
11 Xie J, Lu YM, Shi JD, Deng XQ, Long W. Visfatin levels in patients with severe pneumonia. World J Emerg Med 2011; 2: 132–136.
12 Papachristou GI, Muddana V, Yadav D, O'Connell M, Sanders MK, Slivka A, et al. Comparison of BISAP, Ranson's, APACHEII, and CTSI scores in predicting organ failure,complications, and mortality in acute pancreatitis. Am J Gastroenterol 2010; 105: 435–441.
13 Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2007; 28: 1462–1536. Epub 2007 Jun 11.
14 Frattola A, Parati G, Cuspidi C, Albini F, Mancia G. Prognostic value of 24-hour blood pressure variability. J Hypertens 1993; 11: 1133–1137.
15 Pierdomenico SD, Di NM, Esposito AL, Di MR, Ballone E, Lapenna D, et al. Prognostic value of different indices of blood pressure variability in hypertensive patients. Am J Hypertens 2009; 22: 842–847.
16 Parati G, Bilo G, Vettorello M, Groppelli A, Maronati A, Tortorici E, et al. Assessment of overall blood pressure variability and its different components. Blood Press Monit 2003; 8:155–159.
17 Steinman L. Elaborate interactions between the immune and nervous systems. Nat Immunol 2004; 5: 575–581.
18 Wang HX, Chen B. Diagnostic role of soluble triggering receptor expressed on myeloid cell-1 in patients with sepsis. World J Emerg Med 2011; 2: 190–194.
19 Waage A, Halstensen A, Espevik T. Association between tumour necrosis factor in serum and fatal outcome in patients with meningococcal disease. Lancet 1987; 1: 355–357.
20 Oberholzer A, Souza SM, Tschoeke SK, Oberholzer C, Abouhamze A, Pribble JP, et al. Plasma cytokine measurements augment prognostic scores as indicators of outcome in patients with severe sepsis. Shock 2005; 23: 488–493.
21 Hotchkiss RS, Coopersmith CM, McDunn JE, Ferguson TA. The sepsis seesaw: tilting toward immunosuppression. Nat Med 2009; 15: 496–497.
22 Hotchkiss RS, Karl IE. The pathophysiology and treatment of sepsis. N Engl J Med 2003; 348: 138–150.
23 Joyner MJ, Charkoudian N, Wallin BG. A sympathetic view of the sympathetic nervous system and human blood pressure regulation. Exp Physiol 2008; 93: 715–724.
24 Charkoudian N, Rabbitts JA. Sympathetic neural mechanisms in human cardiovascular health and disease. Mayo Clin Proc 2009; 84: 822–830.
25 Cowley AW Jr, Liard JF, Guyton AC. Role of the baroreceptor reflex in daily control of arterial blood pressure and other variables in dogs. Circ Res 1973; 32: 564–576.
Received April 23, 2013
Accepted after revision September 3, 2013
World J Emerg Med 2014;5(1):42–47
10.5847/ wjem.j.issn.1920–8642.2014.01.007
杂志排行
World journal of emergency medicine的其它文章
- Wilderness medicine
- Lean techniques for the improvement of patients'flow in emergency department
- The knowledge level offinal year undergraduate health science students and medical interns about cardiopulmonary resuscitation at a university teaching hospital of Northwest Ethiopia
- Strategic planning and designing of a hospital disaster manual in a tertiary care, teaching, research and referral institute in India
- Effects of early rehabilitation therapy on patients with mechanical ventilation
- Bispectral index in predicting the prognosis of patients with coma in intensive care unit
