Possible Role of Mast Cells and Neuropeptides in the Recovery Process of Dextran Sulfate Sodium-induced Colitis in Rats△
2013-11-18PingZhaoLeiDongJinyanLuoHaitaoGuanHuiMaandXueqinWang
Ping Zhao*,Lei Dong,Jin-yan Luo,Hai-tao Guan,Hui Ma,and Xue-qin Wang
Department of Gastroenterology,The Second Affiliated Hospital of Xi’an Jiaotong University Medical College,Xi’an 710004,China
ULCERATIVE colitis (UC) is a chronic non-specific type of colitis,of which the etiological factors and pathogenesis are not completely clear.Several studies have shown that the number of mast cells (MCs),which abound in the gastrointestinal tract in normal condition and have been implicated in diverse homeostatic functions,is elevated in the intestinal tissue of patients with UC.1Increasing attention has been paid to the role of MCs in the pathogenesis of UC.In addition,many reports have shown that UC patients demonstrate a derangement of a variety of gut hormones,a group of peptide hormones that exist both in the central nervous system and the gastrointestinal tract.2This study observed the variation of MCs and 3 types of gut horomones including substance P (SP),vasoactive intestinal peptide (VIP),and somatostatin (SS) at different phases of dextran sulfate sodium (DSS)-induced colitis in rats.
MATERIALS AND METHODS
Materials
Twenty-five male Sprague-Dawley (SD) rats weighing 180-200 g were provided by the experimental animal center of Xi’an Jiaotong University.DSS (molecular weight 5000) was produced by Sigma Co.,Ltd.(Munich,Germany);rabbit anti-SP polyclonal antibody by Biomol(Farmingdale,NY,USA);rabbit anti-VIP polyclonal antibody and rabbit anti-SS polyclonal antibody by Santa Cruz(Dallas,TX,USA);SP,VIP,and SS radioimmunoassay kits were bought from the radioimmunity navy center.Streptavidin-biotin-peroxidase complex (SABC) kits and polylysine were bought from Wuhan Boster Biological Technology,Ltd.
Experimental procedures
The 25 male SD rats were randomly separated into a DSS group (n=20) and a control group (n=5).In the DSS group,colitis was induced by putting 4% DSS solution in drinking water for 7 days,and then the 4% DSS solution was replaced by water for 10 days.Rats in the control group drank water during the study period and were sacrificed at the beginning of the experiment.3,4The rats in the DSS group were separately sacrificed on day 8,day 13,and day 18.
Counting of MCs in the colon
The abdomens of the rats in the DSS group were opened after anesthetization with 20% urethane on days 8,13,and 18.After observation of the gross appearance,the colon was opened along the mesenteric side.Then a 1.5-cm section of the distal colon which covered normal,inflammatory,and ulcerative areas was cut.The samples of the colon were fixed with 10% formaldehyde solution,cut into sections,and stained with hematoxylin and eosin for observation of inflammation,and toluidine blue for MCs observation.Sections stained with hematoxylin and eosin were used for histological examination.The number of MCs per millimeter of serosa-sided tissue in the vertical crosssection was then counted under a microscope.
Measurement of histamine in blood and colon
To measure histamine in blood,2.8 mL of deionized water was added to 0.5 mL of heparin-anticoagulated whole blood until complete hemolysis;0.7 mL 25% trichloroacetic acid was then slowly added.After centrifugation at 1780 ×gfor 10 minutes,the supernatant was collected and stored at-80°C.
To measure histamine in colon,4 mL of 25% trichloroacetic acid was added to 100 mg distal segment of colon tissue.The solution was then grinded repeatedly into a homogenate.After centrifugation at 1780 ×gfor 10 minutes,the supernatant was collected and stored at-80°C.The concentrations of histamine in blood and colon tissue were measured using fluorescence method.
Immunohistochemistry of SP,VIP,and SS
Following deparaffinization and rehydration,the paraffin sections were incubated in 3% H2O2at room temperature for 10 minutes to inhibit endogenous peroxidase.The sections were digested with combined alimentary juice for 10 minutes (for VIP staining) or boiled in 0.01 mol/L citric acid buffer (pH 6.0) for 20 minutes (for SP and SS staining).The sections were saturated with non-immune goat serum for 30 minutes at room temperature.Primary antibodies were then applied against SP (rabbit anti-SP polyclonal antibody,1∶8000),VIP (rabbit anti-VIP polyclonal antibody,1∶200),or SS (rabbit anti-SS polyclonal antibody,1∶200).After the sections were incubated overnight at 4°C in a humidified chamber,avidin-labeled secondary antibody and SABC were separately applied to the sections for 30 minutes at room temperature.The sections were then reacted in 3,3’-diaminobenzidine-containing solution for 1-3 minutes and counterstained with hematoxylin.Sections of rat jejunum tissue were used as a positive control.The sections not incubated with primary antibodies served as positive control.
Radioimmunoassay of SP,VIP,and SS
For the radioimmunoassay,100 mg distal colon tissue was boiled in 1 mL normal saline for 3 minutes followed by homogenization in 0.5 mL of 0.1 mol/L hydrochloric acid.The homogenate was kept at 4°C for 2 hours,mixed with 0.5 mL of 0.1 mol/L NaOH,and centrifuged for 10 minutes at 957.6 ×gat 4°C.The supernatant was aspirated and stored at -80°C.The levels of SP,VIP,and SS in the colon tissue were determined using commercial competitive radioimmunoassay kits.
Statistical analysis
All the statistical analysis was performed using SPSS version 12.0.The data were presented as means ±SD.The significant difference between means was determined using one-way analysis of variance for comparisons.P<0.05 was considered statistically significant.
RESULTS
Gross changes of colon with DSS-induced colitis at different periods
On day 8,the colon of DSS rats was shortened,thickened,and obviously rigid with mucosa appearing hyperemic,edematous,anabrotic,and ulcerated.The changes were more severe at the ileocecal junction and the distal colon.The irregular ulcers and anabrosis in the distal colon were diffuse but predominately within 3-4 cm of the anal canal(Fig.1A).Histological examination of the colonic sections revealed that the inflammation primarily involved the mucosa and submucosa,some superficial epithelium had sloughed off,intraepithelial caliciform cells were decreased,and that normal crypt architecture was lost.Infiltrative inflammatory cells were primarily neutrophils(Fig.1B,1C).On day 13,the colon injury recovered to some extent,but the local hyperemia,edema,and ulceration of the mucosa in the colon remained.Regeneration of the epithelium,hyperplasia of the glands,and crypt loss were observed.On day 18,the ulcers in colon were healed,but the mucosa still showed local hyperemia and edema.Histological examination revealed that the colon mucosa was almost entirely healed,and few inflammatory cells were observed.
Changes in MCs count during healing of DSS-induced colitis
In normal rats,MCs were mainly distributed in the mucosa and submucosa,especially in the lamina propria,occasionally in the serosa and never in the muscularis propria.MCs were often near small blood vessels and exhibited a slight degranulation phenomenon (Fig.2A).Histological observation of the DSS group on day 8 showed that the number of MCs increased significantly in the distal colon (P<0.05,Table 1).MCs were mainly distributed in the mucosa and submucosa,especially in the lamina propria,and showed a tendency to accumulate around dilated small vessels,exhibiting obvious degranulation (Fig.2B).The number of MCs was still increased significantly on day 13 (P<0.05,Table 1),and the degranulation of MCs remained.By the time of day 18,the number of MCs in the distal colon dropped back to normal,and there was only slight degranulation.
Variation of histamine level in blood and colon during healing of DSS-induced colitis
On day 8,the histamine level in whole blood increased significantly in the DSS group (P<0.01),while the histamine level in the distal colon mucosa decreased (P<0.05)(Table 1).On day 13 and day 18,the levels of histamine in whole blood and distal colon mucosa both gradually restored to normal.
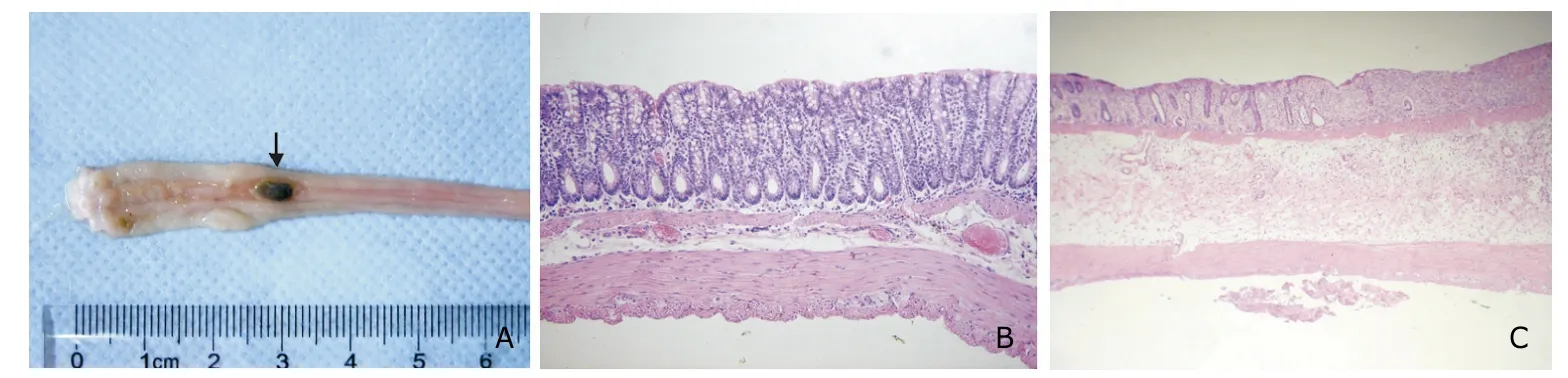
Figure 1.Gross morphological and histopathological changes in rat colon.
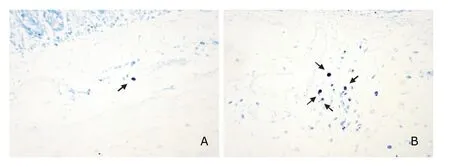
Figure 2.The distribution of mast cells (arrows) in rat colon tissue (toluidin blue ×200).

Table 1.Changes in mast cells (MCs) count in the distal colon,and histamine level in whole blood and colo atdifferent periods of DSS-induced ulcerative colitis§
Immunohistochemical staining and radioimmunoassay results of SP,VIP,and SS in different periods of DSS-induced colitis
The SP,VIP,and SS immuno-reaction positive nerve fibers were buffy and localized in the lamina propria,muscular layer,and myenteric plexus,with the apperance of spots,curves,or clusters.Some distinctly positive cells were also observed.The SP-positive nerve fibers in the distal colon of the DSS group were increased in number,thicker and more densely stained than in the control group,which were most apparent on day 13 (Fig.3A,B).On day 18,the amount and density of SP-positive nerve fibers in the distal colon restored to normal.The density and distribution of VIP-positive and SS-positive nerve fibers in the distal colon did not change as significantly as SP-positive nerve fibers at different periods (Fig.3C-F).
On day 8,the level of SP in the distal colon of the DSS group increased slightly,but with no significant difference.The concentration of SP in the distal colon increased rapidly on day 13 (P<0.05,Table 2),and the concentration of SP restored to normal levels by day 18.The levels of VIP and SS did not demonstrate such significant changes during the different periods.
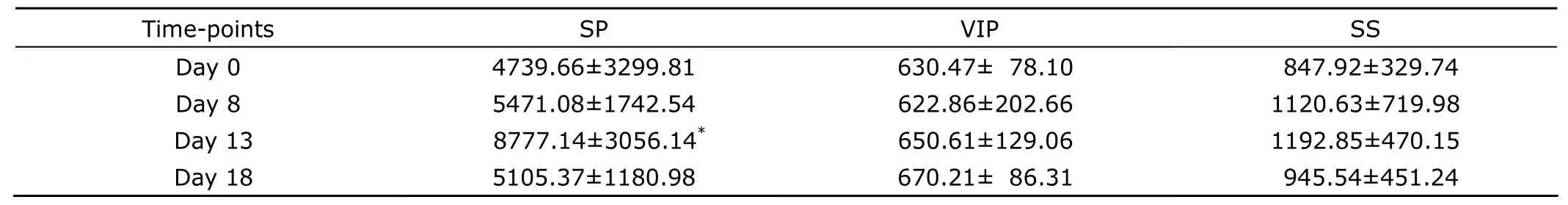
Table 2.Changes in SP,VIP,and SS levels in the distal colon at different periods of DSS-induced ulceratic colitis (pg/mL)§
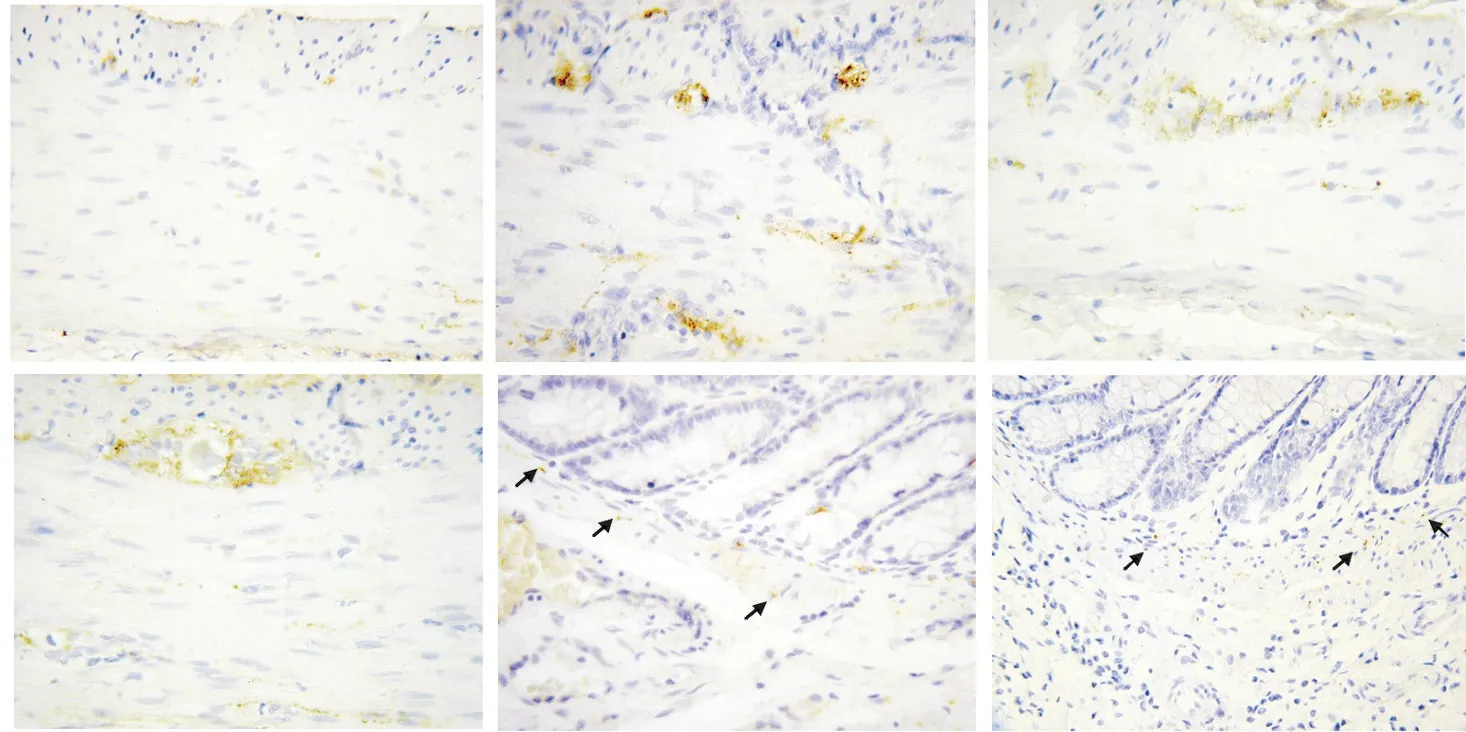
Figure 3.The distribution of SP-,VIP-,and SS-positive nerve fibers and nerve plexus (arrows) in rat colon (hematoxylin ×200).
DISCUSSION
This study revealed that the number of MCs increased significantly during the acute phase of DSS-induced colitis in rats,and that MCs are mainly distributed in the mucosa and submucosa,especially in the lamina propria,accumulated around dilated small vessels with obvious degranulation.These findings relates the pathogenesis of UC to over-activation of MCs,as previously stated.5As a type of cells abundant in the gastrointestinal tract,MCs have been implicated in diverse homeostatic functions and play a critical role in allergic and other inflammatory statuses through releasing multifunctional mediators and cytokines,such as histamine and proteinases.6This study showed that in the acute stage of DSS-induced rat colitis,the histamine concentration in colonic tissue is significantly lower than that in the control group (P<0.05),whereas the whole blood histamine level was obviously higher than that in the control group (P<0.01),indicating that MCs directly participate in the mucosa injury process of DSS-induced rat colitis by releasing histamine.It is now believed that the activated MCs release several mediators,cytokines,and chemokines,which can influence the inflammation process of the gastrointestinal tract and participate in the development of UC.7
In this study,the concentration of SP increased in the distal colon at different periods of DSS-induced colitis,in accordance with the findings of prior reports.8SP can modulate important functions of the intestinal tract,such as mucosa permeability,motility,chloride secretion,and inflammation induced by the activation of cyclooxygenase-2,prostaglandin E2,and nuclear factor-κB.9-11It has been reported that SP levels in the serum and colonic mucosa of UC patients are significantly higher than those in healthy individuals.SP-positive nerve fibers are thicker,more densely stained and more widely distributed in UC patients.12,13The elevation of SP levels in UC patients is probably related to an increase in SP synthesis rather than to the regeneration of intestinal neurons.Increased SP synthesis leads to a higher visibility of SP-positive nerve fibers,hence more SP-positive nerve fibers in UC patients than in healthy controls.14The functions of SP is modulated through its receptor.It has the strongest binding ability with neurokinin-1 receptor (NK-1R),which has a much higher expression level in the colons of UC patients compared with healthy individuals.15ViaNK-1R,SP promotes intestinal fibrogenesis after chronic colitis by stimulating fibrotic responses in fibroblasts.16Animal experiments with mice have shown that NK-1R antagonists abrogates the watery diarrhea,and results in significantly reduction in colonic patch hypertrophy,leukocyte recruitment,tissue damage,SP level in the colon,and total MCs numbers in the colon in dinitrofluorobenzene-induced colitis,demonstrating that SP and NK-1R play an important role in the pathogenesis of UC.17SP can promote the degranulation of MCs through receptor-independent mechanisms and induce MCs to release bioactive compounds.18The results of this study indicated that during the process of DSS-induced colitis,the increase in histamine level in the whole blood and the number of MCs in the distal colon occurred before the increase in SP level in the distal colon,suggesting that activated MCs promote SP release from the adjoining nerve endings through releasing multifunctional mediators.
The present study detected no change in the VIP level in the distal colon at different phase of DSS-induced rat UC.Previous reports have shown that plasma VIP levels do not change in UC,nor in the colonic mucosa and submucosa in UC.19,20The effect of VIP in the pathogenesis of UC needs further study to clarify.Similarly,this study demonstrated no change in the SS level in the distal colon of DSS-induced rat UC at different phases.It was reported that plasma SS level increased significantly during the active UC stage compared with the normal phase,whereas the level in the colon remained normal or decreased in the active UC stage.21
In conclusion,the results of this study suggest that MCs degranulation followed by histamine release plays an important role in the pathogenesis of DSS-induced UC.By releasing multifunctional mediators,activated MCs may promote SP release from the adjacent nerve endings,which in turn may participate in the progression of inflammation and the recovery of DSS-induced UC.The effect of MCs and gut hormones in the pathogenesis of UC needs further study.
1.Nishida Y,Murase K,Isomoto H,et al.Different distribution of mast cells and macrophages in colonic mucosa of patients with collagenous colitis and inflammatory bowel disease.Hepatogastroenterology 2002;49∶678-82.
2.Gross KJ,Pothoulakis C.Role of neuropeptides in inflammatory bowel disease.Inflamm Bowel Dis 2007;13∶918-32.
3.Márquez L,Pérez-Nievas BG,Gárate I,et al.Anti-inflammatory effects of Mangifera indica L.extract in a model of colitis.World J Gastroenterol 2010;16∶4922-31.
4.Zhao P,Dong L,Luo JY,et al.Establishment of dextran sulfate sodium-induced ulcerative colitis model in rats.J Fourth Mil Med Univ 2005;26∶1738-40.
5.Wallon C,Persborn M,Jönsson M,et al.Eosinophils express muscarinic receptors and corticotropin-releasing factor to disrupt the mucosal barrier in ulcerative colitis.Gastroenterology 2011;140∶1597-607.
6.Hodges K,Kennedy L,Meng F,et al.Mast cells,disease and gastrointestinal cancer∶A comprehensive review of recent findings.Transl Gastrointest Cancer 2012;1∶138-50.
7.Wierzbicki M,Brzezińska-Błaszczyk E.The role of mast cells in the development of inflammatory bowel diseases.Postepy Hig Med Dosw (Online) 2008;62∶642-50.
8.Verma-Gandhu M,Verdu EF,Bercik P,et al.Visceral pain perception is determined by the duration of colitis and associated neuropeptide expression in the mouse.Gut 2007;56∶358-64.
9.Koon HW,Zhao D,Xu H,et al.Substance P-mediated expression of the pro-angiogenic factor CCN1 modulates the course of colitis.Am J Pathol 2008;173∶400-10.
10.Liu L,Shang F,Morgan MJ,et al.Cyclooxygenasedependent alterations in substance P-mediated contractility and tachykinin NK1 receptor expression in the colonic circular muscle of patients with slow transit constipation.J Pharmacol Exp Ther 2009;329∶282-9.
11.Koon HW,Zhao D,Zhan Y,et al.Substance P stimulates cyclooxygenase-2 and prostaglandin E2 expression through JAK-STAT activation in human colonic epithelial cells.J Immunol 2006;176∶5050-9.
12.Tavano F,di Mola FF,Latiano A,et al.Neuroimmune interactions in patients with inflammatory bowel diseases∶disease activity and clinical behavior based on substance P serum levels.J Crohns Colitis 2012;6∶563-70.
13.Watanabe T,Kubota Y,Muto T.Substance P containing nerve fibers in ulcerative colitis.Int J Colorectal Dis 1998;13∶61-7.
14.Vento P,Kiviluoto T,Keränen U,et al.Quantitative comparison of growth-associated protein-43 and substance P in ulcerative colitis.J Histochem Cytochem 2001;49∶749-58.
15.ter Beek WP,Biemond I,Muller ES,et al.Substance P receptor expression in patients with inflammatory bowel disease.Determination by three different techniques,i.e.,storage phosphor autoradiography,RT-PCR and immunohistochemistry.Neuropeptides 2007;41∶301-6.
16.Koon HW,Shih D,Karagiannides I,et al.Substance P modulates colitis-associated fibrosis.Am J Pathol 2010;177∶2300-9.
17.Rijnierse A,van Zijl KM,Koster AS,et al.Beneficial effect of tachykinin NK1 receptor antagonism in the development of hapten-induced colitis in mice.Eur J Pharmacol 2006;548∶150-7.
18.Kulka M,Sheen CH,Tancowny BP,et al.Neuropeptides activate human mast cell degranulation and chemokine production.Immunology 2008;123∶398-410.
19.Lee CM,Kumar RK,Lubowski DZ,et al.Neuropeptides and nerve growth in inflammatory bowel diseases∶a quantitative immunohistochemical study.Dig Dis Sci 2002;47∶495-502.
20.Baticic L,Detel D,Kucic N,et al.Neuroimmunomodulative properties of dipeptidyl peptidase IV/CD26 in a TNBSinduced model of colitis in mice.J Cell Biochem 2011;112∶3322-33.
21.Schepens MA,Vink C,Schonewille AJ,et al.Dietary heme adversely affects experimental colitis in rats,despite heat-shock protein induction.Nutrition 2011;27∶590-7.
杂志排行
Chinese Medical Sciences Journal的其它文章
- Effect of Nitric Oxide on Esophageal Cancer Cell Line TE-1
- Clinical Study on Suspension Pancreatic-Duct-Jejunum End-to-Side Continuous Suture Anastomosis in Pancreaticoduodenectomy
- Awareness of Cornea Donation of Registered Tissue Donors in Nanjing△
- Breast Milk Lead and Cadmium Levels in Suburban Areas of Nanjing,China
- Effect of Phenylephrine on Alveolar Fluid Clearance in Ventilator-induced Lung Injury△
- Arthroscopic Debridement and Synovium Resection for Inflammatory Hip Arthritis