Modi fied frontolateral partial laryngectomy operation:combined muscle-pedicle hyoid bone and thyrohyoid membrane flap in laryngeal reconstruction
2013-09-26DianOuyangTianRunLiuYanFengChenJianWang
Dian Ouyang, Tian-Run Liu, Yan-Feng Chen, Jian Wang
1Key Laboratory of Oncology in Southern China, Guangzhou 510060, China; 2Department of Head and Neck, Sun Yat-sen University Cancer Center, Guangzhou 510060, China; 3Department of Otorinolaryngology Head and Neck Surgery, The Sixth Affiliated Hospital of Sun Yat-sen University, Guangzhou 510655, China; 4Department of Anesthesia, Sun Yat-Sen University Cancer Center, Guangzhou 510060, China
Introduction
Laryngeal reconstruction after extensive vertical partial or frontal partial laryngectomy is often challenging.Several reconstruction techniques have been reported.Based on these methods, we considered that a technique using a combined muscle-pedicle hyoid bone and thyrohyoid membrane flap might provide a bony structural support for the remaining thyroid cartilage framework.This technique could also be used for mucosal repair with the fascial thyrohyoid membrane.
Laryngeal reconstruction may be classi fied in different groups,including laryngeal lumen resurfacing and maintenance as well as glottic and vestibular reconstruction.Different flaps and grafts have been used to construct intraluminal prostheses and skinflaps, mucosal flaps, skin and mucosal grafts, perichondrium and muscle flaps, and cartilage flaps1-8.A muscle-pedicle hyoid bone flap is commonly used in laryngeal reconstruction after vertical partial or frontal partial laryngectomy.The first use of a hyoid bone to repair laryngotracheal stenosis was reported by Looper in 19389.In 1960, Bennett et al.10used an autologous hyoid bone graft to treat subglottic stenosis.Alonso et al.11also used a hyoid bone in their experimental study of dogs in 1975.Finnegan12was the first to report the use of a hyoid bone combined with a muscle-pedicle flap in dogs.Ward et al.13used a muscle-pedicle hyoid bone flap to treat laryngotracheal stenosis.In 2004, Cansiz14used a muscle-pedicle hyoid bone flap to repair laryngotracheal stenosis in 23 patients.However, these studies have revealed a risk of laryngeal stenosis (or failure of reconstruction) ranging from 4% to 32%.
We considered that a muscle-pedicle hyoid bone could provide an effective bony structural support.However, we need to determine whether or not the use of a hyoid bone flap can improve the success rate of reconstruction after vertical partial or frontal partial laryngectomy.The ideal laryngeal reconstruction provides a firm framework to maintain the airway and facilitate re-epithelialization in the laryngeal cavity1.Hence, we combined a muscle-pedicle chimeric thyrohyoid membrane with a hyoid bone.The use of the thyrohyoid membrane as local fascia may prevent excessive granulation.In this study, the surgical technique was demonstrated and the results were discussed.
Patients and methods
Patients
The research ethics board of the Sun Yat-Sen University Cancer Center approved the study.All of the participants provided a written informed consent.Four male patients (median age 62 years, ranging from 51 to 76 years) underwent the proposed procedure between August 2008 and November 2009.Their clinical features are summarized in Table 1.Case one had an anterior commissure and glottic tumors that extended to the subglottis and impaired vocal mobility.This case was defined preoperatively as stage T2but was upstaged to T4abecause the cricothyroid membrane was invaded.In case two, glottic tumors were restaged as rT1bafter the patient failed to respond to radiotherapy and then upstaged to rT3because of a minor erosion of the thyroid cartilage.Case three classified as stage T3had a glottic tumor extending to the paraglottic space with impaired vocal mobility; anterior commissure was also observed.Case four classi fied as stage T4ahad a subglottic tumor invading cricoid and cricothyroid membranes with normal vocal mobility and anterior commissure.Pathological examination confirmed the diagnosis of a well-differentiated squamous cell laryngeal carcinoma in these four cases.Preoperative examination,including physical examination, laryngoscopy, high-resolution computed tomography or magnetic resonance imaging, and pulmonary function tests were performed in accordance with the NCCN Clinical Practice Guidelines in Head and Neck Cancer 2008.
Operative technique
Laryngectomy phase
Two types of laryngeal framework defects were commonly observed after tumor resection: type A, which was observed after extensive frontal/vertical partial laryngectomy without partial resection of the cricoid cartilage; and type B, which was observed after extensive frontal/vertical partial laryngectomy,including partial resection of the cricoid cartilage (Figure 1).
During the procedure, strap muscles were exposed and separated carefully to expose the anterior laryngotracheal wall.Considering the location and the extent of the tumor,the thyroid cartilage was split vertically on the healthy side by using microsaws approximately 5 mm from the edge of the tumor.The frontal partial trachea was cut transversely along the upper edge of the first ring of the trachea (0.5 cm under the edge of the tumor).The incision was curved upward and proceeded vertically to connect to the incision in the thyroid cartilage.The thyroepiglottic ligament was then cut transversely along the upper edge of the thyroid cartilage.The frontal partial laryngeal soft tissue covering the tumor was dissected with the frontal thyroid cartilage on both sides.In the laryngeal cavity,the incision was made at a safe margin of 0.5 cm from the edgeof the tumor.If necessary, all of the fold card and the arytenoid cartilage were removed with the tumor.During resection, the thyrohyoid membrane was reserved.Delphian lymph node was removed from the patients and subjected to pathological analysis.Selective lateral neck dissection (levels II, III, and IV)was performed in cases with T3or T4alaryngeal cancer revealing a clinically negative neck.
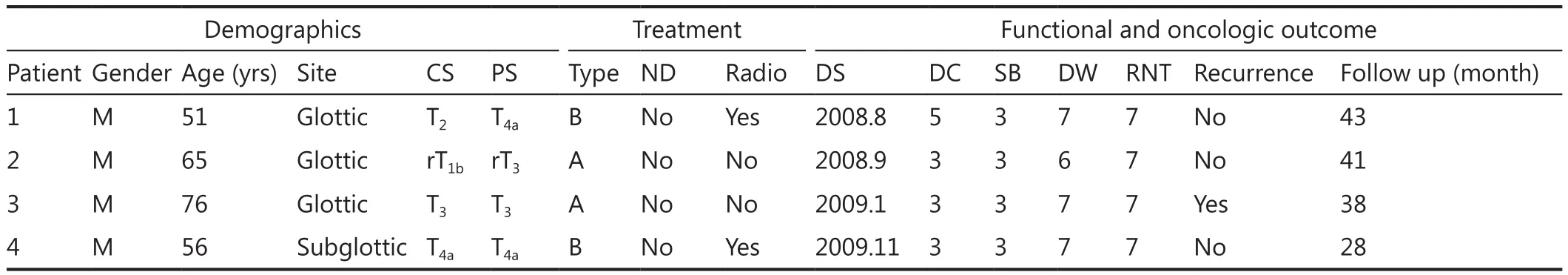
Table 1 Clinical data of patients

Figure 1 Surgical defect of the larynx after extensive partial laryngectomy.Type A, extended frontal/vertical partial laryngectomy without partial resection of the cricoid cartilage.Type B, extended frontal/vertical partial laryngectomy with partial resection of the cricoid cartilage (frontal partial resection of the cricoid cartilage based on Type A).
Harvesting flap
The combined muscle-pedicle hyoid bone and thyrohyoid flap should include the hyoid bone with its blood supply, the hyothyroid membrane, and the infrahyoid muscles.The pedicle is an inferior part connected to the upper edge of the thyroid cartilage and the pre-epiglottic space.The suprahyoid muscles were cut along the upper edge of the hyoid bone.The lesser cornu and the greater cornu were cut from the body of the hyoid bone.The infrahyoid muscles and the hyothyroid membrane were kept attached to the hyoid bone and to the upper edge of the thyroid cartilage.The thyrohyoid membrane is a broad,fibroelastic layer attached to the upper border of the thyroid cartilage and the upper margin of the posterior surface of the body and the greater cornua of the hyoid bone.This membrane facilitates the upward movement of the larynx during deglutition.To maintain blood supply, the aforementioned structures were separated from the level of the hyoid body down to the upper edge of the thyroid cartilage.The periosteum and the blood supply of these structures were retained.The flap attached to the upper edge of the thyroid cartilage, which is the origin of the flap pedicle, was also retained.
Bone fixation
The shoulder pads were removed and the neck was maintained at a supine position.The body of the hyoid bone, pedicled with the attached hyothyroid membrane and infrahyoid muscles, was turned down and attached to the remaining cartilage framework to obtain a stable bony support.In type A defects, the hyoid bone was attached on the remaining thyroid cartilage at the vocal cord level (Figure 2).In type B defects, the hyoid bone was attached to the remaining cricoid cartilage (Figure 3).Microsaws were used to create peripheral openings, attaching the bony graft to the thyroid or the cricoid cartilage with nonabsorbable 2-0 Prolene sutures (Ethicon, Johnson & Johnson Medical, Livingston, UK).The hyoid bone was fixed in a bridgelike fashion across the cricothyroid cartilage edges (Figure 2).The laryngeal cavity was slightly expanded when fixing to ensure that the new cartilage framework was stable and provide ventilation for the larynx.
Repair of laryngeal mucosal defect

Figure 2 Combined hyoid bone flap in laryngeal framework reconstruction: type A.The hyoid bone was fixed in the glottic position above the remaining thyroid cartilage.A.Surgical view; B.Mortise view; C.Lateral view.
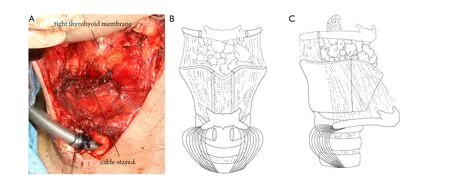
Figure 3 Combined hyoid bone flap in laryngeal framework reconstruction: type B.The hyoid bone was fixed to the remaining cricoid cartilage.A.Surgical view; B.Mortise view; C.Lateral view.
The thyrohyoid membrane, a tough fibroelastic ligament attached to the superior margin of the thyroid cartilage and adjacent to the lower border of the hyoid bone, was flipped over to cover the frontal laryngeal defect in the same way as one flips the pages of a book.The hyoid bone was placed across the remaining laryngeal cartilages.The hyothyroid membrane should be kept relatively tight because a loose membrane may drop into the laryngeal cavity under negative pressure during ventilation, and this incident may lead to laryngostenosis.The remaining defects were then partially covered above the membrane with the infrahyoid muscle.Quicksetting fibrin glue (Tissucol, Immuno, Austria) was used as a sealant.A drain (non-suction type) was placed subcutaneously.
In type A cases (Figure 2), supraglottic defects were repaired using the thyrohyoid membrane.Subglottic defects were repaired using the infrahyoid muscle.Glottic defects were closed using the hyoid bone.In type B cases, glottic defects were mainly repaired with the thyrohyoid membrane, and the subglottic defects were covered with the infrahyoid muscle and the hyoid bone (Figure 3).
Preoperative and postoperative assessment
The following outcome measures were prospectively recorded:morbidity and mortality (complications), oncological safety, and functional outcome.
Results
Functional outcome
No patient had postoperative dyspnea or dysphagia.No patient died during the postoperative course.The four patients received voice training very early after the procedure.Their vocal qualities were raspy and slightly deeper compared with their preoperative condition.The volume was weak when they made a call.The shortterm functional recovery of the patients was normal (Table 1).
Potential surgery-related complications
No postoperative failure of healing caused by wound infection,seroma, major subcutaneous emphysema, laryngocele,hematoma, cervical skin necrosis, laryngeal chondritis with fistula formation, laryngeal stenosis, or secondary stenosis was observed in any of the four patients.
Oncologic results
The follow-up periods for the four patients were 43, 41, 38, and 28 months, respectively.Case one, case two and case four did not suffer from tumor recurrence during the follow-up period.Case three underwent total laryngectomy because of tumor recurrence in the paraglottic space, but no evidence of further tumor recurrence was found at the final assessment.
Discussion
With developments in chemoradiotherapy, laser resection,and transoral robotic surgery, partial laryngectomy has not been considered as the preferred method but remains a good alternative technique of organ preservation protocols.The procedure usually provides good local control of diseases and a satisfactory functional outcome15-17.However, partial laryngectomy is mainly recommended for selected patients with T3or T4atumor in glottic or subglottic area.
Tucker et al.18used the epiglottis in laryngeal cavity reconstruction because the epiglottis provides support for the laryngeal cavity and inhibits excessive local granulation, thereby preventing laryngostenosis.However, this type of reconstruction alters the normal position of the epiglottis and impairs swallowing.By contrast, the use of a combined muscle-pedicle hyoid bone flap in laryngeal reconstruction provides support for the laryngeal cavity and prevents altering the position of the epiglottis.As a result, epiglottic function and swallowing are preserved.The major feature of our technique involves the use of the thyrohyoid membrane to repair laryngeal mucosa defect19.As a type of fascia, the thyrohyoid membrane has numerous advantages compared with other grafts20,21.This membrane is sufficiently large to cover defects of various sizes, easy to prepare,and adaptable to recipient sites.The thyrohyoid membrane is also resistant to saliva, infection, motion, and irradiation;this procedure also provides a high survival rate because the membrane is poorly vascularized and has low metabolism22-24.The combined muscle-pedicle hyoid bone and thyrohyoid membrane flap, as a chimeric flap, prevents excessive local granulation, thereby reducing the incidence of laryngotracheal stenosis, compared with muscle-pedicle hyoid bone flaps.This combination is a reliable graft to perform one-stage repair of laryngotracheal defects, providing effective repair of the mucosa and cartilage support.
In 2004, Cansiz et al.14reported the use of muscle-pedicle hyoid bone flaps (without the thyrohyoid membrane) to reconstruct laryngeal or tracheal defects.Furthermore, four offive cases with T3laryngeal carcinoma and 14 of 17 cases with laryngotracheal stenosis were decannulated at an average of 21.4 days after reconstruction.After decannulation, their respiration, speech quality, and swallowing were adequate.However, three patients (3/23, 13.6%) suffered from laryngotracheal stenosis after reconstruction.In our study,the short-term functional recovery of the four patients was normal.No patient died during the postoperative course.No postoperative dyspnea, dysphagia, and failure of healing caused by wound infection, cervical skin necrosis, or laryngeal stenosis were observed in any of the patients.Three patients did not suffer from tumor recurrence during the follow-up period.The mean duration of tracheostomy tube (3.5 d) and the nasogastric tube(7 d) in our study were shorter than those in the report of Cansiz et al.14.
The current study is a case series study describing a technique performed on only four patients; however, procedure-related complications and functional outcomes were expected.This outcome may be attributed to several advantages: (1) The hyoid bone has a high survival rate25because a stable blood supply is well preserved in the flap; (2) The hyoid bone is sufficiently long to have a large cross-section that supports an extended laryngeal cavity for ventilation26,27; (3) The epiglottis is retained in place without “pull down” and its function is preserved; the same results are observed in the arytenoids and the cricoarytenoid joints.The cricoarytenoid unit relies on the action of the cricoarytenoid joint, which allows the arytenoid cartilage to function; (4) The use of a thyrohyoid membrane flap to reconstruct the frontal lateral laryngeal cavity prevents excessive local granulation.The thyrohyoid membrane flap is also sufficiently long to repair defects of the thyroid cartilage and the cricothyroid membrane; (5) Reconstruction does not affect the outcome of postoperative radiotherapy.In our patient series, two patients who received postoperative radiotherapy had satisfactory survival and few complications.
However, the technique also has limitations.The flap is suitable for patients who have undergone extensive vertical partial laryngectomy or frontal partial laryngectomy.At least the posterior one-third of the bilateral thyroid ala or the posterior half of the cricoid cartilage should be preserved to perform hyoid bone fixation and create a bony support for the laryngeal cavity.The pre-epiglottic space should be free of tumor to repair the mucosal defect of the thyrohyoid membrane.Laryngotracheal defect should also be limited above the level of the first tracheal ring, which is limited by the length of the thyrohyoid.
Conclusion
The combined muscle-pedicle hyoid bone and thyrohyoid membrane flap is a reliable graft that can be used in one-stage repair of laryngotracheal defects, providing a cartilage support and an effective repair of the mucosa.Vocal quality, swallowing function, and ventilation after the procedure were favorable.However, the number of cases in this study was very small to perform statistical analysis.A large sample should be enrolled in future studies to further evaluate the importance of this flap.
This study was supported by the Natural Science Foundation of Guangdong Province, China (Grant No.303041353002).
Conflict of interest statement
No potential conflicts of interest are disclosed.
1.Guerra AB, Miller LA, Soueid NE, Metzinger SE.Laryngotracheal reconstruction using a rigidly fixated split clavicular myoosseous flap: a 10-year review.Ann Plast Surg 2006;57:402-407.
2.McCaffrey TV.Management of laryngotracheal stenosis on the basis of site and severity.Otolaryngol Head Neck Surg 1993;109(3 Pt 1):468-473.
3.McCaffrey TV.Classi fication of laryngotracheal stenosis.Laryngoscope 1992;102:1335-1340.
4.Service RF.Tissue engineering.Coming soon to a knee near you:cartilage like your very own.Science 2008;322:1460-1461.
5.Genden EM, Govindaraj S.Allograft tracheoplasty technique for management of refractory tracheal stenosis.Ann Otol Rhinol Laryngol 2006;115:302-305.
6.Cotton RT.Management of subglottic stenosis.Otolaryngol Clin North Am 2000;33:111-130.
7.Langer R, Vacanti JP.Tissue engineering.Science 1993;260:920-926.
8.Neville WE, Bolanowski JP, Kotia GG.Clinical experience with the silicone tracheal prosthesis.J Thorac Cardiovasc Surg 1990;99:604-612; discussion 612-613.
9.Looper EA, Lyon IB.Laryngeal tuberculosis; observations based on an experience of 28 years with laryngeal tuberculosis.Ann Otol Rhinol Laryngol 1948;57:754-768.
10.Bennett T.Laryngeal strictures.South Med J 1960;53:1101-1104.
11.Alonso WA, Druck NS, Griffiths CM, Sumner HW, Ogura JH.Cricoid arch replacement in dogs.Further studies.Arch Otolaryngol 1975;101:42-45.
12.Finnegan DA, Wong ML, Kashima HK.Hyoid autograft repair of chronic subglottic stenosis.Ann Otol Rhinol Laryngol 1975;84:643-649.
13.Ward PH, Canalis R, Fee W, Smith G.Composite hyoid sternohyoid muscle grafts in humans.Its use in reconstruction of subglottic stenosis and the anterior tracheal wall.Arch Otolaryngol 1977;103:531-534.
14.Cansiz H, Yener HM, Sekercioglu N, Günes M.Laryngotracheal reconstruction with a muscle-pedicle hyoid bone flap: a series of 23 patients.Ear Nose Throat J 2004;83:424-427.
15.Nibu K, Kamata S, Kawabata K, Nakamizo M, Nigauri T, Hoki K.Partial laryngectomy in the treatment of radiation-failure of early glottic carcinoma.Head Neck 1997;19:116-120.
16.Hartl DM, Landry G, Hans S, Marandas P, Brasnu DF.Organ preservation surgery for laryngeal squamous cell carcinoma:Low incidence of thyroid cartilage invasion.Laryngoscope 2010;120:1173-1176.
17.Ganly I, Patel SG, Matsuo J, Singh B, Kraus DH, Boyle JO, et al.Results of surgical salvage after failure of de finitive radiation therapy for early-stage squamous cell carcinoma of the glottic larynx.Arch Otolaryngol Head Neck Surg 2006;132:59-66.
18.Tucker HM, Wood BG, Levine H, Katz R.Glottic reconstruction after near total laryngectomy.Laryngoscope 1979;89:609-618.
19.Oysu C, Aslan I.Cricohyoidoepiglottopexy vs near-total laryngectomy with epiglottic reconstruction in the treatment of early glottic carcinoma.Arch Otolaryngol Head Neck Surg 2006;132:1065-1068.
20.Soerdjbalie-Maikoe V, van Rijn RR.Embryology, normal anatomy,and imaging techniques of the hyoid and larynx with respect to forensic purposes: a review article.Forensic Sci Med Pathol 2008;4:132-139.
21.Apostolopoulos K, Samaan R, Labropoulou E.Experience with vertical partial laryngectomy with special reference to laryngeal reconstruction with cervical fascia.J Laryngol Otol 2002;116:19-23.
22.Dursun G, Ozgursoy OB.Laryngeal reconstruction by platysma myofascial flap after vertical partial laryngectomy.Head Neck 2005;27:762-770.
23.Eló J, Horváth E, Késmárszky R.A new method for reconstruction of the larynx after vertical partial resections.Eur Arch Otorhinolaryngol 2000;257:212-215.
24.Lim YC, Son EJ, Kim K, Kim KM, Choi EC.Perichondrial flap to prevent chondritis and cartilage necrosis in salvage vertical partial laryngectomy for recurrent glottic carcinoma after irradiation: a new procedure.Acta Otolaryngol 2005;125:659-663.
25.Alonso WA, Druck NS, Ogura JH.Clinical experiences in hyoid arch transposition.Laryngoscope 1976;86:617-624.
26.Miller KW, Walker PL, O’Halloran RL.Age and sexrelated variation in hyoid bone morphology.J Forensic Sci 1998;43:1138-1143.
27.Huang WC, Chen HC, Wei FC, Cheng MH, Schnur DP.Chimeric flap in clinical use.Clin Plast Surg 2003;30:457-467.
杂志排行
Cancer Biology & Medicine的其它文章
- Clinicopathologic characteristics and prognostic factors of 63 gastric cancer patients with metachronous ovarian metastasis
- A survey and evaluation of population-based screening for gastric cancer
- Research progress in the radioprotective effect of the canonical Wnt pathway
- Preoperative intestinal stent decompression with primary laparoscopic surgery to treat left-sided colorectal cancer with obstruction: a report of 21 cases
- Erratum to research development of the relationship between thymidine phosphorylase expression and colorectal carcinoma