Effects of resistance and Tai Ji training on mobility and symptoms in knee osteoarthritis patients
2013-06-21MihlWortlySongningZhngMximPquttErinByrLusBumgrtnrGryKlipplJohnKrusnklusLrryBrown
Mihl Wortly,Songning Zhng,Mxim Pqutt,Erin Byr,Lus Bumgrtnr, Gry Klippl,John Krusnklus,Lrry Brown
aPellessippi State Community College,Knoxville,TN 37932,USA
bDepartment of Kinesiology,Recreation and Sport Studies,The University of Tennessee,Knoxville,TN 37996,USA
cDepartment of Health&Sport Sciences,University of Memphis,Memphis,TN 38152,USA
dDepartment of Rheumatology,The University of Tennessee Medical Center,Knoxville,TN 37920,USA
eTennessee Sports Medicine Group,Knoxville,TN 37919,USA
Original article
Effects of resistance and Tai Ji training on mobility and symptoms in knee osteoarthritis patients
Michael Wortleya,Songning Zhangb,*,Maxime Paquettec,Erin Byrdb,Lucas Baumgartnerb, Gary Klippled,John Krusenklause,Larry Brownb
aPellessippi State Community College,Knoxville,TN 37932,USA
bDepartment of Kinesiology,Recreation and Sport Studies,The University of Tennessee,Knoxville,TN 37996,USA
cDepartment of Health&Sport Sciences,University of Memphis,Memphis,TN 38152,USA
dDepartment of Rheumatology,The University of Tennessee Medical Center,Knoxville,TN 37920,USA
eTennessee Sports Medicine Group,Knoxville,TN 37919,USA
Background:No studies have compared effectiveness of resistance training and Tai Ji exercise on relieving symptoms of knee osteoarthritis (OA).The purpose of the study was to evaluate effects of a 10-week Tai Ji and resistance training intervention on improving OA symptoms and mobility in seniors with knee OA.
Methods:Thirty-one seniors(60—85 years)were randomly assigned to a Tai Ji program(n=12),a resistance training program(n=13),and a control group(n=6).All participants completed the Western Ontario and McMaster(WOMAC)Osteoarthritis Index and performed three physical performance tests(6-min walk,timed-up-and-go,and timed stair climb and descent)before and after the 10-week intervention.
Results:The participants in the resistance training group significantly improved on the timed-up-and-go test(p=0.001),the WOMAC pain subscore(p=0.006),WOMAC stiffness sub-score(p<0.001),and WOMAC physical function sub-score(p=0.011).The Tai Ji group significantly improved on the timed-up-and-go test(p<0.001),but not on the WOMAC scores.
Conclusion:Resistance training was effective for improving mobility and improving the symptoms of knee OA.Tai Ji was also effective for improving mobility,but did not improve knee OA symptoms.
Copyright©2013,Shanghai University of Sport.Production and hosting by Elsevier B.V.All rights reserved.
Knee;Osteoarthritis;Resistance training;Tai Chi;Tai Ji
1.Introduction
Osteoarthritis(OA)is the leading cause of disability in the United States.1OA causes pain and stiffness in the affected joint,and can also lead to a decline in knee strength and slowing of gait speed beyond what is normally expected due to advancing age.2These changes often result in significant limitation of daily activities for people with knee OA and consequently lead to the loss of functional independence. Lawrence et al.1estimated that in 2005,18.6 million U.S. citizens over 60 years old had mild,moderate,or severe radiographic knee OA,of which about 6 million were clinically symptomatic.
Many forms of exercise,including walking,resistance training,hydrotherapy,flexibilitytraining,andbalancetraining, have been investigated as potential methods of managing OA symptoms and improving mobility.3,4Resistance training hasbeen shown to improve strength and mobility in elderly populations,5—7and to improve strength and physical function of knee OA patients without increasing knee pain.8,9Some studies have reported that resistance training also helped reduce pain associatedwithOA.10—13IntheOsteoarthritisResearchSociety International(OARSI)recommendations for managing knee OA,Zhang et al.14reported a small effect size for knee strengthening for both reducing pain(95%CI 0.23—0.42)and improving function(95%CI 0.23—0.41).However,reports of the effectiveness of resistance training to reduce OA symptoms vary widely,although the effects are typically positive.
Tai Ji(also referred as Tai Chi),a 4-century-old Chinese martial art and a mind—body therapy,is characterized by many slow and flowing movements with graceful and gentle transition from one to the other.15,16It has gained increasing popularity as an OA treatment.A growing number of randomized and controlled clinical trials in the past 20 years have found that participation in Tai Ji can improve quality of life and physical function.17It has been demonstrated that Tai Ji improves balance,strength,flexibility,cardiovascular and respiratory functions,pain,depression,anxiety,and arthritic symptoms in various populations.18Some studies have found an improvement in pain19,20in knee OA populations,while others have found this change was not significantly different from control subjects.21Only a handful of randomized clinical trials evaluating Tai Ji for OA have been conducted,22and the evidence for the effectiveness of Tai Ji is mixed.
The objective of this study was to evaluate and compare the effectiveness of a 10-week Tai Ji intervention and a 10-week resistance training intervention in senior citizens with knee OA.Each intervention was evaluated in terms of its ability to improve strength and mobility,and to reduce pain and stiffness resulting from knee OA.It was hypothesized that both interventions would equally improve the mobility and OA symptoms of the participants.
2.Methods
2.1.Participants
Participants were recruited from Knox county area senior centers,advertisement in local newspaper and a local newsletter for seniors.Interested persons were asked to contact the researchers by telephone,and all callers were given a brief telephone interview to see if they met the inclusion and exclusion criteria(Fig.1).To be eligible to participate,the callers had to be between the ages of 60 and 85 years,and have knee OA.Participants were excluded if they had received arthroscopic surgery or an intra-articular injection within the past 3 months,neurological disorders,or had participated in a resistance training or Tai Ji in the past 6 months.Potential participants who met the pre-screening criteria were invited to a screening session conducted by one of the co-authors to confirm that participants met the clinical inclusion criteria based on the Classification Criteria for Knee OA of the American College of Rheumatology.23Finally,bilateral knee X-rays were taken and evaluated for osteophytes and joint space narrowing by the same co-author based on the Kellgren/ Lawrence(K/L)scale.24Individuals with a K/L grade between 1 and 4 of the medial knee compartment and petellofemoral joint were included in the study.All participants read and signed an informed consent document approved by the Institutional Review Boards.

Fig.1.Flow-chart of study protocol.
All qualified participants attended a baseline data collection session(Fig.1).During the data collection session,each participant completed a Physical Activity Scale for the Elderly (PASE)survey25in order to monitor their overall level of activity.All participants performed tests to evaluate the participant’s mobility,OA symptoms,and gait.The baseline data collection was conducted within a 2-week period prior to the intervention program.Following the 10-week intervention, all participants completed a post-training data collection session identical to the baseline session within a 2-week period.The pre-and post-training tests were conducted by the same researchers.
2.2.Intervention
Within two weeks of completing the baseline testing session the participants were pseudo-randomly assigned to either a resistance training program(RT),a Tai Ji program (TJ),or a control group(CON)based on gender and pain score of the Western Ontario and McMaster(WOMAC)Osteoarthritis Index.26All three groups were asked not to alter their regular physical activity or pain medications during the 10-week intervention programs.
The RT group participated in an open-kinetic chain resistance training program designed specifically for knee OA patients,which consisted of two 1-h sessions per week.The program included the following knee and hip exercises performed with ankle cuff weights:seated leg extension,standing hamstring curl,straight leg raise,standing hip abduction, standing hip adduction,standing hip flexion,standing calf raise.Participants started with either a 5 lb or 10 lb ankle weight and progressed from two sets of eight repetitions tothree sets of 12 repetitions during the first 6 weeks,and were allowed to increase the weight as needed during the final 4 weeks.
The TJ group participated in a 1-h group training session twice per week in which they learned and practiced a program of 12 basic movements adapted from the Yang style Tai Ji.The program was designed by a Tai Ji master with 35 years of experience.The program began by learning the first two movements during the first session,and then adding a new movement during each session for the first 5 weeks.In each training session of the first weeks,sufficient time was provided for practicing the new and previously learned movements. During the last 5 weeks,participants also practiced the movements in the opposite direction to the original direction in order to similarly“load”both lower limbs.
The CON group was asked not to alter their usual physical activity or medication during the 10 weeks of the intervention, and was contacted once by telephone during the intervention.
2.3.Tests of mobility and symptoms
To evaluate mobility associated with walking,stair ascent/ descent,and chair rise,participants performed three physical function tests at the baseline and post-training test sessions. The 6-min walk test(6MWT)was conducted on a 49 m×2 m rectangle hallway that was marked with painter’s tape on the floor.The participants were instructed to walk around the rectangle in order to cover as much ground as possible in 6 min,27and the distance walked was measured to the nearest tenth of a meter.In the timed-up-and-go test(TUG),participants were timed as they rose from an arm chair,walked 3 m, turned around,and then walked back to the chair and sat down.28Three trials of the TUG test were performed and the average time was used for data analysis.During the timed stair climb and descent(SCD),the participants were timed as they climbed a single flight of 11 stairs,turned around,and descended the same flight of stairs at a quick but safe speed. The subjects were instructed that they could use the hand rails for support,but not for pushing or pulling their way up the stairs.28Because participants often found this activity painful, it was only performed once.
The WOMAC questionnaire(Visual analog scale version 3.1)was administered at the baseline and post-training testing sessions.In addition,the WOMAC was also administered at the end of the 5th week of the training sessions only for the RT and TJ groups.The sub-scales of pain,stiffness,and physical function of WOMAC were used as dependent variables.
2.4.Statistical analysis
The baseline and post-training values for the participants’body mass index(BMI)and PASE scores,as well as the dependent variables,were compared using a 3× 2(group ×time)mixed model analysis of variance(ANOVA)with time as a repeated factor(18.0 SPSS;Chicago,IL,USA).Paired samplettests were performed if the group×time interaction or the time main effect were significant.The alpha level for all statistical tests was set at 0.05 a priori.Pvalues between 0.05 and 0.10 were considered marginally significant.The K/L grades are scored on an ordinal scale and were analyzed using a non-parametric Kruskal—Wallis test(p<0.05).
3.Results
3.1.Participants
Thirty-one out of 39 participants who started the study completed the study.The participants who did not complete the intervention did not differ from the other participants in age,height,or mass.No differences were found between groups at baseline for any variable(Table 1).The attendance rates were 87.69%and 81.67%for the RT and TJ groups, respectively.
There was a significant group× time interaction for the PASE scores(F(2,28)=5.560,p=0.009,observed power (OP)=0.81).Thepost hoccomparison indicated no difference between the baseline and follow-up PASE scores for the CON group,but the post-training PASE scores were signif icantly greater than baseline for both the RT(p<0.001)and the TJ(p=0.032)groups(Table 1).
Although the groups were balanced on their baseline WOMAC pain scores,the groups did have different distributions of K/L grades,with all four participants with a K/L grade of 4 being in the TJ group.The Kruskal—Wallis test of the K/L grades,however,found no significant difference between the three groups.
3.2.Mobility
There were no significant differences for the 6MWT. There was a significant main effect for time on the TUG test(F(1,28)=31.935,p<0.001,OP=1.00,Table2).Thepost hoctest found that TUG times were significantly faster posttrainingforboththe RT(p=0.001)andTJgroups(p<0.001), butonly a marginal difference for CON(p=0.088).Therewas a marginally significant time effect for SCD(F(1,28)=3.486,p=0.072,OP=0.44).Post hoccomparisons showed marginally significantpre/postdifferencesforthe RT group(p=0.071)andtheTJgroup(p=0.061).Effectsizes(Cohen’sd)29of training for the physical function tests were provided in Table 2.
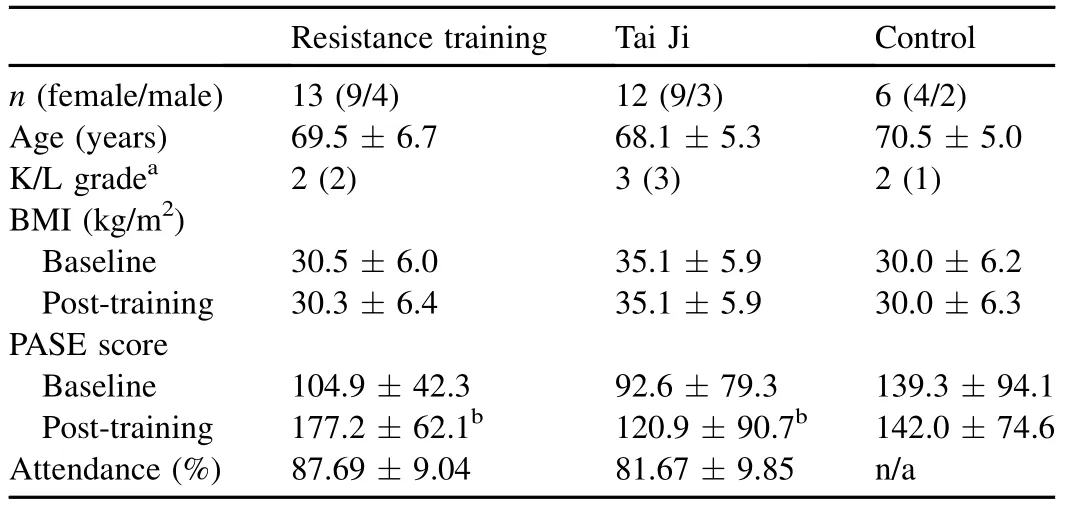
Table 1 Participant and training group information(mean±SD).

Table 2 Mobility test results at baseline and post-training(mean±SD).
3.3.Knee OA symptoms
TheANOVAsontheWOMAC sub-scalesshowed a marginally significant time effect on the pain sub-scale(F(1, 28)=4.130,p=0.052,OP=0.50,Table 3).Paired-samplettests showed a significant improvement on the pain sub-scale (p=0.006)forthe RTgroup,butnotfortheTJ orCON groups. There were both a significant time effect(F(1,28)=7.187,p=0.012,OP=0.74)and interaction(F(2,28)=4.482,p=0.020,OP=0.72)for the stiffness sub-scale.Post hoccomparisons showed a significant improvement on the stiffness sub-scale(p<0.001)for the RT group,but not for the TJ or CON groups.For the physical function sub-scale,there was a significanttimeeffect(F(1,28)=4.726,p=0.038,OP=0.56).Post hoccomparisons for the physical function sub-scale were significant for the RT group(p=0.011),but not for the other groups.Effect sizes of training for the WOMAC sub-scales were provided in Table 3.
4.Discussion
The results of this study demonstrate that both the resistance training and Tai Ji training programs were effective in improving mobility of the participants.The RT group improved by16%onTUGand21%onSCD,whiletheTJgroupimproved by 12%and 11%on the TUG and SCD,respectively.Also,both groups had moderate to large effect sizes for both the TUG (effect size:-0.68 for TJ and-0.80 for RT)and SCD(effect size:-0.77 for TJ and-0.90 for RT)compared to the control group,which are in line with values reported in the literature. Effect sizes calculated from data reported in a study of participants ina12-week 24-formTai Chiforarthritis classwere2.46 and 2.52 for the TUG and RT tests,respectively.21The participants in a resistance training program improved their TUG by 10%,andparticipantsinTaiJiimprovedby12%,4bothofwhich aresimilartotheimprovementsfoundinthisstudy.Toppetal.12reported improvements of their participants in stair ascending and descending performance by approximately 15%after a program of resistance training and pain medication,while the resistance training participants in this study improved by 20.8%.The lack of improvement in 6MWT may be related to the nature of the two training programs.The 6MWT is more aerobic in nature than the TUG and SCD,and neither interventionwasdesignedtoimprovetheaerobiccapacity.However, both training groups showed significant improvements in the TUGtestandmarginalimprovementsinSCDtest.Theseresults showed some evidence of improvements in gait speed.
The resistance training intervention in this study appears to have been effective at improving WOMAC scores.Although the time main effect for the pain sub-scale was only marginally significant,theRThadalargeeffectonimprovingbothpainand stiffness(ES=-0.86 and-1.16,respectively)and a moderate effect for physical function(ES=-0.58).Estimates of effect size in the literature for pain,stiffness,and physical function range from-0.21,-0.18,and-0.25 respectively30to-3.17, -2.74,and-3.58.12The OARSI recommendations for management of knee OAalsolisted positiveeffect sizesof knee strengthening as 0.32 for both improvement of pain and physical function.14In addition,Fig.2 shows the changes in the WOMAC sub-scales from baseline to post-training,including an intermediate point that the participants completed after 5 weeks of training(not included in statistical comparisons). Most of the improvements made by the RT group seemed to occur in the first 5 weeks of training.

Table 3 WOMAC sub-scale scores at baseline and post-training(mean±SD).
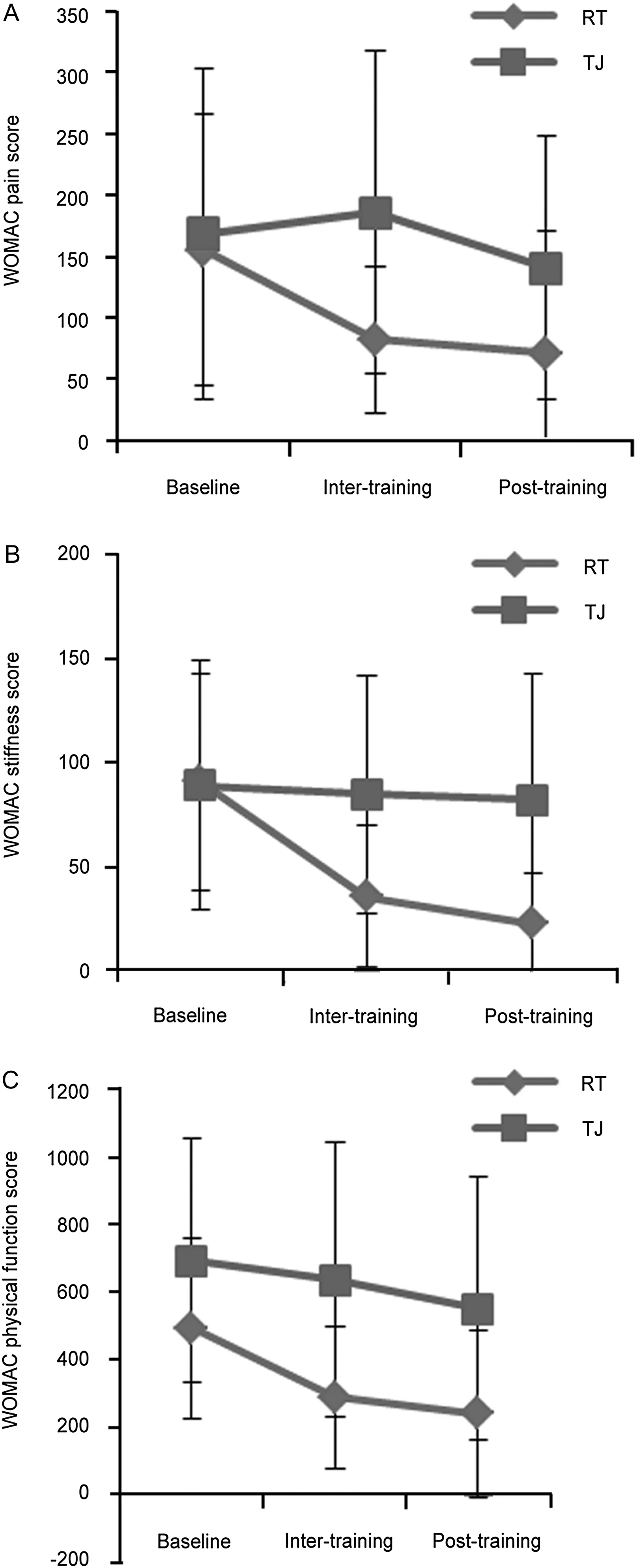
Fig.2.Comparison of the change in Western Ontario and McMaster (WOMAC)Osteoarthritis Index scores between resistance training(RT)and Tai Ji(TJ)groups.(A):WOMAC pain sub-scale;(B):WOMAC stiffness subscale;(C):WOMAC physical function sub-scale.
The results of this study suggest that the Tai Ji intervention had little-to-no effect on the participants’OA symptoms reflected in the WOMAC sub-scale scores.This finding is contrary to some of Tai Ji intervention literature.For example, the participants of another study had significant improvements on both the pain and physical function sub-scales that were also significantly different from the control group beginning at week 9 during a 12-week intervention.19There was also a significant difference from baseline in the stiffness sub-score which was not significantly different from controls.A Tai Ji intervention study by Fransen et al.21found a significant improvement of 9.7(on a 100-point scale)on the physical function sub-scale beyond the control group,which was considered to be of moderate clinical significance.They did not find significant differences on the WOMAC pain subscale.The lack of significant improvement on the WOMAC in this study could be due to the short duration of the Tai Ji intervention(10 weeks).Another potential reason for the lack of improvement is that four of the 12 participants in the TJ group had a K/L grade of 4,which may have predisposed the TJ group to improving more slowly.
Of the two interventions,the open-kinetic chain resistance training with ankle weights appears to be the more promising therapy for people with knee OA.Although it was not specifically addressed in this study,there could be a simple underlying mechanism that makes open-kinetic chain resistance training better for knee OA than closed-chain exercises and other weight bearing activities.It is known that metabolism of cartilage depends partly on its mechanical environment.31,32In a closed-kinetic chain activity,such as Tai Ji,the peak quadriceps activation and peak tibiofemoral contact forces occur when the knee is flexed.33During an open-kinetic chain exercise,peak tibiofemoral contact force occurs when the knee is fully extended.33When the knee is flexed in the open-kinetic chain exercises,the ankle weight is essentially pulling the knee into traction.This mechanical difference could explain why the RT group in this study saw an improvement when some other studies have not.Further research is warranted to determine if open-kinetic chain resistance training can result in changes in cartilage health, measured through either MRI imaging or biomarkers.
The small size of the control group,which began with nine participants but finished with six due to participants’dropout, may limit the ability to detect differences between the two training groups and the control group.Another limitation is that all of the K/L grade 4 patients were assigned to the Tai Ji intervention since K/L grades were not available at the time of group assignments.Although the difference in K/L was not statistically significant,the Tai Ji group did have a higher median K/L grade which may have delayed improvements in the TJ group compared to the RT group.Another limitation is that the TJ group spent up to 5 weeks to learn all 12 movements and may not have experienced the full benefits of training with 12 movements and the equal amount of“exposure”as the RT group,although participants were provided sufficient time to practice the new and previously learned movements during the first 5 weeks.
5.Conclusion
Both open-kinetic chain resistance training and Tai Ji were effective in improving the timed-up-and-go and stair climb and descend performance in seniors with knee OA.However, little-to-no improvement in the WOMAC scores were found for Tai Ji group,while resistance training showed a large effect size for reducing both WOMAC pain and stiffness scores and a moderate effect on WOMAC physical function scores. Further research is warranted to determine if open-kinetic chain resistance training can be effective at relieving OA symptoms for a broader population of OA patients,and to see if Tai Ji could be effective at relieving OA symptoms in populations with mild OA.
Acknowledgments
We would like to acknowledge the John O’Connor Senior Center and Frank R.Strang Senior Center for allowing and assisting us to conduct the training sessions at their facility,and allparticipantsfortheirparticipationsinthestudy.Thisstudywas supportedinpartbyfundsfromUTKOfficeofResearch,College of Education,Health and Human Sciences,and University of Tennessee Medical Center,The University of Tennessee.
1.Lawrence RC,Felson DT,Helmick CG,Arnold LM,Choi H,Deyo RA, et al.Estimates of the prevalence of arthritis and other rheumatic conditions in the United States.Part II.Arthritis Rheum2008;58:26—35.
2.Go¨k H,Ergin S,Yavuzer G.Kinetic and kinematic characteristics of gait in patients with medial knee arthrosis.Acta Orthop Scand2002;73:647—52.
3.Burks K.Osteoarthritis in older adults:current treatments.J Gerontol Nurs2005;31:11—9.
4.Takeshima N,Rogers NL,Rogers ME,Islam MM,Koizumi D,Lee S. Functional fitness gain varies in older adults depending on exercise mode.Med Sci Sports Exerc2007;39:2036—43.
5.Fiatarone MA,Marks EC,Ryan ND,Meredith CN,Lipsitz LA,Evans WJ. High-intensity strength training in nonagenarians.Effects on skeletal muscle.J Am Med Assoc1990;263:3029—34.
6.Judge JO,Underwood M,Gennosa T.Exercise to improve gait velocity in older persons.Arch Phys Med Rehabil1993;74:400—6.
7.Manini T,Marko M,VanArnam T,Cook S,Fernhall B,Burke J,et al. Efficacy of resistance and task-specific exercise in older adults who modify tasks of everyday life.J Gerontol A Biol Sci Med Sci2007;62:616—23.
8.Huang MH,Lin YS,Yang RC,Lee CL.A comparison of various therapeutic exercises on the functional status of patients with knee osteoarthritis.Semin Arthritis Rheum2003;32:398—406.
9.King LK,Birmingham TB,Kean CO,Jones IC,Bryant DM,Giffin JR. Resistance training for medial compartment knee osteoarthritis and malalignment.Med Sci Sports Exerc2008;40:1376—84.
10.Ettinger Jr WH,Burns R,Messier SP,Applegate W,Rejeski WJ, Morgan T,et al.A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis.The Fitness Arthritis and Seniors Trial(FAST).J Am Med Assoc1997;277:25—31.
11.Gu¨r H,Cakin N,Akova B,Okay E,Ku¨c¸u¨koˇglu S.Concentric versus combined concentric-eccentric isokinetic training:effects on functional capacity and symptoms in patients with osteoarthrosis of the knee.Arch Phys Med Rehabil2002;83:308—16.
12.Topp R,Woolley S,Hornyak 3rd J,Khuder S,Kahaleh B.The effect of dynamic versus isometric resistance training on pain and functioning among adults with osteoarthritis of the knee.Arch Phys Med Rehabil2002;83:1187—95.
13.Roddy E,Zhang W,Doherty M.Aerobic walking or strengthening exercise for osteoarthritis of the knee?A systematic review.Ann Rheum Dis2005;64:544—8.
14.ZhangW,MoskowitzRW,NukiG,AbramsonS,AltmanRD,ArdenN,etal. OARSIrecommendationsforthemanagementofhipandkneeosteoarthritis, part I:critical appraisal of existing treatment guidelines and systematic review of current research evidence.Osteoarthr Cartil2007;15:981—1000.
15.Hong Y,Li JX.Biomechanics of Tai Chi:a review.Sports Biomech2007;6:453—64.
16.Wang C,Schmid CH,Hibberd PL,Kalish R,Roubenoff R,Rones R,et al. Tai Chi for treating knee osteoarthritis:designing a long-term follow up randomized controlled trial.BMC Musculoskelet Disord2008;9:108, http://dx.doi.org/10.1186/1471-2474-9-108.
17.Klein PJ,Adams WD.Comprehensive therapeutic benefits of Taiji: a critical review.Am J Phys Med Rehabil2004;83:735—45.
18.Wang C,Collet JP,Lau J.The effect of Tai Chi on health outcomes in patients with chronic conditions:a systematic review.Arch Intern Med2004;164:493—501.
19.Brisme´e JM,Paige RL,Chyu MC,Boatright JD,Hagar JM,McCaleb JA, et al.Group and home-based tai chi in elderly subjects with knee osteoarthritis:a randomized controlled trial.Clin Rehabil2007;21:99—111.
20.Song R,Lee EO,Lam P,Bae SC.Effects of tai chi exercise on pain, balance,muscle strength,and perceived difficulties in physical functioning in older women with osteoarthritis:a randomized clinical trial.J Rheumatol2003;30:2039—44.
21.Fransen M,Nairn L,Winstanley J,Lam P,Edmonds J.Physical activity for osteoarthritis management:a randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes.Arthritis Rheum2007;57:407—14.
22.Lee MS,Pittler MH,Ernst E.Tai chi for osteoarthritis:a systematic review.Clin Rheumatol2008;27:211—8.
23.Altman R,Asch E,Bloch D,Bole G,Borenstein D,Brandt K,et al. Development of criteria for the classification and reporting of osteoarthritis.classification of osteoarthritis of the knee.Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association.Arthritis Rheum1986;29:1039—49.
24.Kellgren JH,Lawrence JS,editors.The epidemiology of chronic rheumatism:atlas of standard radiographs of arthritis.Oxford:Blackwell Scientific;1963.
25.Washburn RA,Smith KW,Jette AM,Janney CA.The Physical Activity Scale for the Elderly(PASE):development and evaluation.J Clin Epidemiol1993;46:153—62.
26.BellamyN,BuchananWW,GoldsmithCH,CampbellJ,StittLW.Validation study of WOMAC:a health status instrument for measuring clinically importantpatientrelevantoutcomestoantirheumaticdrugtherapyinpatients with osteoarthritis of the hip or knee.J Rheumatol1988;15:1833—40.
27.Enright PL,McBurnie MA,Bittner V,Tracy RP,McNamara R,Arnold A, et al.The 6-min walk test:a quick measure of functional status in elderly adults.Chest2003;123:387—98.
28.Kennedy DM,Stratford PW,Wessel J,Gollish JD,Penney D.Assessing stability and change of four performance measures:a longitudinal study evaluating outcome following total hip and knee arthroplasty.BMC Musculoskelet Disord2005;6:3.
29.Cohen J.Statistical power analysis for the behavioral sciences.New York: Academic Press;1969.
30.Thomas KS,Muir KR,Doherty M,Jones AC,O’Reilly SC,Bassey EJ. Home based exercise programme for knee pain and knee osteoarthritis: randomised controlled trial.BMJ2002;325:752.
31.Andriacchi TP,Mu¨ndermann A,Smith RL,Alexander EJ,Dyrby CO, Koo S.A framework for thein vivopathomechanics of osteoarthritis at the knee.Ann Biomed Eng2004;32:447—57.
32.Guilak F,Fermor B,Keefe FJ,Kraus VB,Olson SA,Pisetsky DS,et al. The role of biomechanics and inflammation in cartilage injury and repair.Clin Orthop Relat Res2004;423:17—26.
33.Escamilla RF,Fleisig GS,Zheng N,Barrentine SW,Wilk KE, Andrews JR.Biomechanics of the knee during closed kinetic chain and open kinetic chain exercises.Med Sci Sports Exerc1998;30:556—69.
24 August 2012;revised 6 December 2012;accepted 28 December 2012
*Corresponding author.
E-mail address:szhang@utk.edu(S.Zhang)
Peer review under responsibility of Shanghai University of Sport
2095-2546/$-see front matter Copyright©2013,Shanghai University of Sport.Production and hosting by Elsevier B.V.All rights reserved. http://dx.doi.org/10.1016/j.jshs.2013.01.001
杂志排行
Journal of Sport and Health Science的其它文章
- Analysis of the TCM theory of traditional Chinese health exercise
- Current concepts in sport concussion management:A multifaceted approach
- Human neuromuscular structure and function in old age:A brief review Geoffrey A.Powera,*,Brian H.Daltonb,Charles L.Ricec,d
- ActiGraph GT3X determined variations in“free-living”standing, lying,and sitting duration among sedentary adults
- Process and outcome evaluation of the“No more smoking!It’s time for physical activity”program
- A 6-week diet and exercise intervention alters metabolic syndrome risk factors in obese Chinese children aged 11—13 years
