Giant neurogenic tumors of mediastinum: report of two cases and literature review
2013-06-12
Department of Thoracic Surgery, Tangshan Gongren Hospital, Tangshan 063000, China
Giant neurogenic tumors of mediastinum: report of two cases and literature review
Jingwei Wang, Jidong Yan, Shuhua Ren, Yu Guo, Yang Gao, Lijun Zhou
Department of Thoracic Surgery, Tangshan Gongren Hospital, Tangshan 063000, China
Corresponding to:Shuhua Ren. Department of Thoracic Surgery, Tangshan Gongren Hospital, Tangshan 063000, China. Email: renshuhua@csco.org.cn.
Neurogenic tumors are commonly found in the mediastinum, especially in the posterior mediastinum or in the chest wall, neurogenic tumors may reach large size before becoming symptomatic. If the neurogenic tumor occupied more than half size of the chest wall accompanied by mediastinal shift, tracheal compression, or superior vena reflux disorder, it may be called giant intrathoracic neurogenic tumors. Giant intrathoracic neurogenic tumors are relatively rare. Most of intrathoracic neurogenic tumors were benign or low-grade malignant tumors in nature. Complete surgical excision should be the rule for these patients. We report two cases of giant neurogenic tumors, and study the clinical manifestations, diagnostic methods, surgical management, and prognosis in the light of the most important published data.
Mediastinal neoplasms; giant intrathoracic neurogenic tumors
Scan to your mobile device or view this article at:http://www.thecjcr.org/article/view/1758/2489
Introduction
Neurogenic tumors are the most common mediastinal tumors, accounting for 12% to 21% of all mediastinal neoplasms (1,2) and 75% to 95% of all posterior mediastinal neoplasms (3). Thoracic neurogenic tumors usually originate from the intrathoracic nerve sheath, autonomic nerve ganglion sections and sub-organizations. Schwannoma is the most common neurogenic tumor. Nearly half of posterior neurogenic tumors are asymptomatic, however, as they become larger in size, they can produce symptoms related to local compression, bone invasion, and spinal cord involvement (4,5). Computed Tomography (CT) and CT-assisted puncture biopsy can improve the quality of preoperative diagnosis. Radical surgery is the method of choice in surgical treatment of giant benign intrathoracic tumors (6). Treatment policy is determined individually on the basis of the results of CT, functional and intraoperative findings.
Case reports
Case 1
A 67-year-old female had a series of symptoms of chest pain, cough, dyspnea, dizziness and palpitation 2 years ago, which were aggravated over the past year. Chest CT (Figure 1) revealed a 16.2 cm × 11.8 cm × 11.0 cm high-density mass with destruction of the bone and huge lesions located in the lower right side of the chest cavity, adjacent to diaphragm. CT value was 76 Hounsfield Unit (HU). Magnetic resonance imaging (MRI) (Figure 2) showed low signal intensity on T1-weighted image, high signal intensity on T2-weighted image, and not remarkably strong intensity on the diffusion weighted imaging. The mass was considered as a neurogenic tumor. In the exploratory thoracotomy view, we found that a huge mass was in the right chest, and densely adhered to the costovertebral region, extending from T5 to T12 and infiltrating part of vertebral bodies of these ribs. In addition, clearly squeezed lungs and pedicled lateral chest wall were observed (Figures 3,4). The duration of operation was 136 mins. Histopathology showed spindle cell neoplasm, with extensive necrosis, moderate mitotic index and severe atypia, probably a malignant peripheral nerve sheath tumor (Figure 5). S-100 protein was positive in immunohistochemical assay, confirming the diagnosis of malignant schwannoma.

Figure 1 CT reveals a huge high-density mass with destruction of the bone and huge lesions located in the lower right side of the chest, adjacent to diaphragm
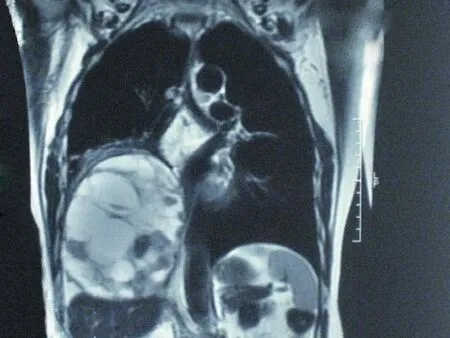
Figure 2 MRI shows low intensity on T1-weighted image, high intensity on T2-weighted image, and not remarkably strong intensity on the diffusion weighted imaging
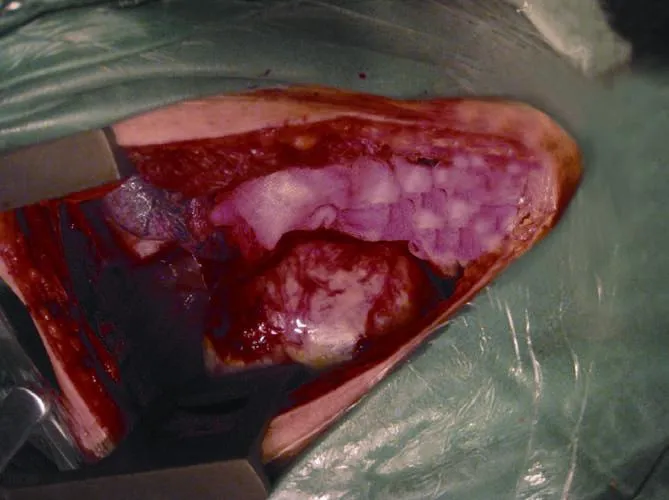
Figure 3 Operative view. A huge mass was in the right chest, and densely adhered to the costovertebral region, extending from T5 to T12
Case 2

Figure 4 Operative specimen
A 53-year-old female patient complained of chest pain for five months. The pain was tolerable in the beginning, whereas it became increasingly intense and accompanied with dyspnea and palpitation. The patient stated that she had no family history of neoplasms and had smoking history of 20 years. A CT scan of the chest revealed an 18.2 cm × 13.8 cm × 8.5 cm well-defined mass, with regular borders and huge lesions located in the left side of the chest, densely adhered to the costovertebral region, and adjacent to thoracic aorta and part of pulmonary artery. CT value was 98 HU. MRI showed high signal intensity on T1-weighted image, and high signal intensity on T2-weighted image. It was a cystic and solid tumor in the left side of the chest cavity, accompanied with internal bleeding and deformation of some vertebral body and pedicle. There was no obvious abnormality of thoracic spinal canal and spinal cord. A left posterolateral thoracotomy was performed after perfect preoperative preparation. Surgical exploration found that the tumor was in the left chest, and hard quality, solid, clear border, and densely adhered to the costovertebral region.The duration of operation was 145 mins. Histopathology showed that some tumor cells were spindle, with round nucleus and blunt ends, and densely arranged, and some other tumor cells were dispersed and sparse, and had reticular cytoplasm with fatty degeneration and many interstitial reticulation or collagen fibers. The glial fibrillary acidic protein (GFAP) was positive in immunohistochemical assay, confirming the diagnosis of neurilemmoma.
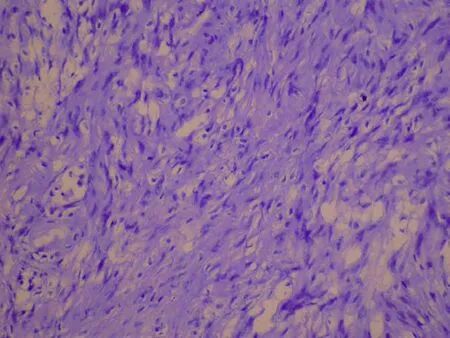
Figure 5 Histopathology shows spindle cell neoplasm, with extensive necrosis, moderate mitotic index and severe atypia, probably a malignant peripheral nerve sheath tumor
Discussion
There was no consensus on clinical diagnostic criteria of giant mediastinal neurogenic tumor. Generally, the neurogenic tumor occupying more than half side of the chest cavity can be called a giant mediastinal neurogenic tumor. In spite of the different clinical features, once diagnosis was established, the mediastinal neurogenic tumors should undergo resection. The clinical manifestations, diagnostic methods, surgical approaches, as well as the principles of surgical treatment and prognosis of primary mediastinal neurogenic tumor are described in details below.
Diagnosis of primary giant mediastinal neurogenic tumor
According to patient’s history, clinical symptoms and signs, and imaging (X-ray, CT or MRI examination), most of primary giant mediastinal neurogenic tumors can be diagnosed. It is very difficult to distinguish tumor from the anterior mediastinum or posterior mediastinum when the giant neurogenic tumor occupies one side of chest cavity. It is very easy to be misdiagnosed as other diseases. The most common presentation in patients is respiratory symptoms with mild chest discomfort, chest pain, irritating cough, chest tightness and shortness of breath. Other symptoms related to local compression, bone invasion, and spinal cord involvement occurred when tumors become larger. Most of mediastinal neurogenic tumors locate in the posterior mediastinum, closing to the spine or paravertebral sulcus, and have smooth and clear boundary and uniform density. Part of tumors may have calcified element (schwannoma, ganglioneuroma, and neuroblastoma), and cystic change (mainly schwannoma). In case of dumbbell tumor, there may be tumor extension into spinal canal and intervertebral enlargement. At present, MRI has more value in evaluating tumor extended into spinal canal than CT. It is difficult to determine benign or malignant according to CT or MRI examination, and the determination of diagnosis mainly relies on pathological examination. Needle biopsy is very important for preoperative pathological diagnosis.
Principles and approaches of surgery, and prognosis of primary giant mediastinal neurogenic tumor
Surgery is the preferred treatment for primary giant mediastinal neurogenic tumor, whether it is benign or malignant. A standard post-lateral thoracotomy can provide a wonderful exposure. Video-assisted thoracic surgery (VATS) is a new technique for mediastinal tumor. VATS minimizes the access trauma and provides an appropriate view, especially for small posterior mediastinal neurogenic tumor (7,8), but it is not suitable for giant mediastinal neurogenic tumor because of huge tumor volume. For dumbbell neurogenic tumors, a sufficient preoperative evaluation of the intraspinal part of the tumor is very important for preventing uncontrollable hemorrhage during the operation. L-shaped incision and cooperation of thoracic surgeon with neurosurgeon are recommended. Benign mediastinal tumor can be cured by surgery. Malignant mediastinal tumor is still one of the least studied topics. The five-year survival rate is low and complete resection is usually impossible. Adjuvant radiotherapy and chemotherapy can be useful in the treatment of the metastatic disease.
In summary, we often encounter some troubles on giant mediastinal neurogenic tumor resection. It is verydifficult to expose clearly because of giant tumor volume in operation. To solve this problem, extending as far as the incision and sternum transaction and bilateral thoracotomy are necessary, and releasing cystic fluid to minimize the tumor volume is practical.
Acknowledgements
Disclosure:The authors declare no conflict of interest.
1. Gholoum S, Fraser R, Ferri LE. Posterior mediastinal chondromatous hamartoma. Ann Thorac Surg 2007;83:1528-30.
2. Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest 2005;128:2893-909.
3. Yamaguchi M, Yoshino I, Fukuyama S, et al. Surgical treatment of neurogenic tumors of the chest. Ann Thorac Cardiovasc Surg 2004;10:148-51.
4. Kumar A, Kumar S, Aggarwal S, et al. Thoracoscopy: the preferred approach for the resection of selected posterior mediastinal tumors. J Laparoendosc Adv Surg Tech A 2002;12:345-53.
5. Saenz NC. Posterior mediastinal neurogenic tumors in infants and children. Semin Pediatr Surg 1999;8:78-84.
6. Strollo DC, Rosado-de-Christenson ML, Jett JR. Primary mediastinal tumors: part II. Tumors of the middle and posterior mediastinum. Chest 1997;112:1344-57.
7. Ng CS, Yim AP. Technical advances in mediastinal surgery: videothoracoscopic approach to posterior mediastinal tumors. Thorac Surg Clin 2010;20:297-309.
8. Cansever L, Kocaturk CI, Cinar HU, et al. Benign posterior mediastinal neurogenic tumors: results of a comparative study into video-assisted thoracic surgery and thoracotomy (13 years’ experience). Thorac Cardiovasc Surg 2010;58:473-5.
Cite this article as:Wang J, Yan J, Ren S, Guo Y, Gao Y, Zhou L. Giant neurogenic tumors of mediastinum: report of two cases and literature review. Chin J Cancer Res 2013;25(2):259-262. doi: 10.3978/j.issn.1000-9604.2013.03.09

10.3978/j.issn.1000-9604.2013.03.09
Submitted Dec 12, 2012. Accepted for publication Jan 08, 2013.
杂志排行
Chinese Journal of Cancer Research的其它文章
- Safety and efficacy of trimodality therapy in patients undergoing extrapleural pneumonectomy
- Treatment of mesothelioma: still a long way to go!
- Role of contrast-enhanced ultrasonography in percutaneous radiofrequency ablation of liver metastases and efficacy evaluation
- Determining the optimal time for bortezomib-based induction chemotherapy followed by autologous hematopoietic stem cell transplant in the treatment of multiple myeloma
- Bevacizumab rescue therapy extends the survival in patients with recurrent malignant glioma
- Bortezomib, dexamethasone plus thalidomide for treatment of newly diagnosed multiple myeloma patients with or without renal impairment
